BACKGROUND
Fibromyalgia (FM) is a chronic and incapacitating disease with high prevalence (Heidari et al., 2017; Queiroz, 2013), a significant social and economic burden (Lacasse et al., 2016), and a multitude of symptoms (Mease et al., 2009) that result in marked deterioration of health-related quality of life (HRQoL) (Hoffman & Dukes, 2008).
The main recognized predictors of a decrease in HRQoL in FM patients are the intensity of clinical symptoms (pain, fatigue and sleep disturbance) (Consoli et al., 2012; Laursen et al., 2005; Oncu et al., 2013; Wagner et al., 2012), as well as anxious and depressive symptoms (Ataoglu et al., 2003; del Pozo-Cruz et al., 2017; Soriano-Maldonado et al., 2015). These affective symptoms (anxiety and depression) not only directly impact HRQoL but can also mediate the influence of clinical pain on physical and mental dimensions of HRQoL (Galvez-Sánchez et al., 2020b). However, there is limited evidence regarding the role of other psychological variables, such as coping strategies and social support, as predictors of HRQoL in patients with FM.
The few studies that have analysed the association between coping strategies and HRQoL in FM have reported varying results. Some studies have found that problem-solving coping strategies have a positive impact on the functioning and HRQoL of FM patients, while emotional-focused coping strategies have the opposite effect (Boehm et al., 2011). Other studies have shown that emotional coping is related to a better HRQoL (Campos & Vázquez, 2012), and in some studies, problem-focused and emotion-focused coping strategies were not significantly associated with HRQoL outcomes, while dysfunctional coping was significantly predictive of poorer physical functioning (Theadom et al., 2007). Recently Galvez-Sánchez et al. (2020a) found that catastrophizing (a negative emotion-focused coping strategy) has a negative impact on HRQoL and mediates the negative influence of pain on several HRQoL domains.
Regarding social support, the majority of studies with FM patients have revealed low social support levels (Gündüz et al., 2019; Montoya et al., 2004). In some studies this low perception of social support has been associated with low HRQoL in FM patients (Da Costa et al., 2000; Freitas et al., 2017), while in others studies this association has not been found (Lee et al., 2017). The small number of studies focused on analysing the relationship between social support and HRQoL and the discrepancy in the results make it necessary to continue research in this area.
Considering simultaneously the effects of anxiety, depression, coping, and social support on HRQoL in FM patients, it is still necessary to expand our understanding of the relationship between these psychological variables and the HRQoL of FM patients and to better understand the interplay and unique contribution of each of these psychological factors in order to improve the overall management and treatment of FM.
The aim of this study was to examine the relationship between anxiety, depression, coping strategies, and social support and HRQoL in patients with FM and to examine through mediation models the role of these psychological variables as a possible indirect mechanism in the association between the clinical variables (pain, fatigue and sleep disturbance) and the physical and mental domains of HRQoL.
PARTICIPANTS AND PROCEDURE
PARTICIPANTS
In a cross-sectional study, we recruited patients with FM who were diagnosed according to the American College of Rheumatology criteria of 1990 (Wolfe et al., 1990) and the American College of Rheumatology criteria of 2010 (Wolfe et al., 2010). Patients were recruited from eight private rheumatology practices, two public rheumatology services, and three chronic pain units in the North of Portugal. The inclusion criteria for this study were as follows: the patients had to be 18 years old or older; have at least one-year evolution since FM diagnosis; and be able to read and write in Portuguese. Patients with physical or cognitive deficit, psychotic disorders and other rheumatic disorders besides FM were excluded from the study.
MEASURES
Sociodemographic and lifestyle data form. Each patient’s sex, age, marital status, educational level completed, self-reported social class, place of residence, employment situation, and body mass index were collected by the psychologist through an individualized interview.
Clinical data form. The referring specialist completed the clinical data form, which included the following information: time since the onset of symptoms, time since diagnosis, time between the onset of symptoms and the diagnosis, number of medical visits due to FM in the last 12 months, and information about pharmacological, complementary, and psychological treatments.
Comorbidity according to the Charlson Comorbidity Index (CCI; Charlson et al., 1987). This instrument assesses the presence of 24 comorbid conditions, with each condition scored between 1 and 6. The scores of each condition are summed to produce a total score.
Brief Physical Activity Assessment Tool (BPAAT; Marshall et al., 2005). This instrument assesses the frequency and duration of physical activities in a “typical” week. The total score ranges from 0 to 8. Patients who score 4 or higher are characterized as sufficiently active, while those who score between 0 and 3 are considered insufficiently active. In this study, we used the Portuguese adaptation of the instrument by Cruz et al. (2021). Both the original and the Portuguese versions have been shown to have suitable psychometric properties (Cruz et al., 2021; Marshall et al., 2005).
McGill Pain Questionnaire (MPQ; Melzack, 1975). It is used to monitor pain resulting in a total score between 0 and 78 points (higher scores are associated with greater pain). In the present study the Portuguese adaptation was used (Kremer et al., 1982; Martins, 1999). The analysis of the data regarding the MPQ dimensions follows the method proposed by Kremer et al. (1982). This instrument presents appropriate psychometric properties (Katz & Melzack, 2011; Melzack, 1987).
Fatigue Severity Scale (FSS; Krupp et al., 1989). It is a self-rated instrument that measures tiredness with nine sentences and a total score between 9 and 63 points (the higher the score, the greater the fatigue). In the present study the Portuguese adaptation was used (Laranjeira, 2012). Both the original and the Portuguese version revealed suitable psychometric properties (Krupp et al., 1989; Laranjeira, 2012; Pereira & Duarte, 2010).
Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989). It is a self-rated instrument used to measure the quality and patterns of sleep in adults. The total score range is 0 to 21 points, with higher scores indicating more sleep problems. The Portuguese adaptation of the PSQI (Bertolazi et al., 2011) was used in this study and has been shown to have satisfactory properties in previous research (Bertolazi et al., 2011; Buysse et al., 1989).
Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983). This questionnaire includes 14 items that are divided into two subscales, each containing 7 items. The purpose is to evaluate anxiety and depression symptoms. Scores for each subscale range from 0 to 21, where a score of 0 to 7 is considered a normal value. Scores between 8 and 10 may indicate possible depression/anxiety, and scores equal to or greater than 11 suggest clinical depression/anxiety. Both the original version and the Portuguese adaptation used in this study (Pais-Ribeiro et al., 2007) have demonstrated good psychometric properties (Pais-Ribeiro et al., 2007; Zigmond & Snaith, 1983).
Brief COPE (Carver, 1997). The instrument measures individual strategies for managing stress and consists of 28 items in 14 subscales. According to Coolidge et al. (2000) coping strategies can be clustered into emotion-focused coping (acceptance, use of emotional social support, humour, positive reinterpretation and religion), problem-focused coping (active coping, instrumental support and the use of planning) and dysfunctional coping (disinvestment behaviour, denial, self-distraction, self-blame, substance use and expression of feelings). In this study, we used the Portuguese adaptation (Pais-Ribeiro & Rodrigues, 2004). Both the original and the Portuguese versions have demonstrated appropriate psychometric properties (Carver, 1997; Pais-Ribeiro & Rodrigues, 2004).
Satisfaction with Social Support Scale (SSSS; Pais-Ribeiro, 1999). The scale is composed of 15 items and four dimensions, including satisfaction with friends, intimacy, satisfaction with family, and social activities. Respondents rate each item on a scale from 1 (totally agree) to 5 (totally disagree). The total score ranges from 15 to 75, with higher scores indicating better perception of social support. The SSSS was specifically designed for the Portuguese population and has demonstrated satisfactory psychometric properties (Pais-Ribeiro, 1999).
Short-Form 36 Health Survey v2 (SF-36v2; Ware, 2000). The questionnaire evaluates generic HRQoL and consists of 36 items that are divided into eight dimensions: physical functioning, physical role functioning, bodily pain, general health, vitality, mental health, social functioning and emotional role functioning. These eight dimensions can be grouped into two components: the physical component summary (PCS) and the mental component summary (MCS). The final scores for each dimension and component range from 0 to 100, with higher scores indicating better health status. In this study we used the Portuguese adaptation of the questionnaire, which demonstrated adequate psychometric properties (Ferreira, 2000a, b).
PROCEDURE
Patients were consecutively selected from private and public rheumatology practices and in chronic pain clinics in the North of Portugal. All patients who met the inclusion criteria, as determined by their physician, were invited to participate in the study. The purposes and procedures of the study were explained to the selected patients, followed by a written informed consent form. The referrer physician completed the clinical data form and the CCI. The psychologist collected information about sociodemographic and lifestyle characteristics through interviews and administered the BPAAT. Patients completed the Fibromyalgia Impact Questionnaire (FIQ) and SF-36v2 questionnaires first, and then the remaining questionnaires (Brief COPE, MPQ, SSSS, HADS, PSQI and FSS) were administered.
The study was approved by the Bioethics Committee of the Santiago de Compostela University, by the Ethics Committee of the Alto Minho Central Hospital, by the Executive Committee of the Braga Central Hospital and by the Ethics Committee of the Alto Ave Central Hospital. The investigation fulfilled the legal requirements regarding data confidentiality and followed the good clinical practices guidelines from the Declaration of Helsinki.
STATISTICAL DESIGN
For the descriptive analysis in this study, the continuous variables were expressed as mean, standard deviation and range, and the categorical variables as frequency and percentage, with the 95% confidence interval estimate.
To quantify the impact of FM on HRQoL the direct scores of the SF-36 were standardized according to the reference values for each decade of age of the general Portuguese population (Ferreira et al., 2012; Ferreira & Santana, 2003). Standardized values are expressed in standard deviations from the mean score of the Portuguese general population of the same age (which would receive the value of 0).
In order to identify the sociodemographic, clinical, and psychological factors associated with HRQoL, univariate analysis was conducted examining the relationship between standardized SF-36v2 scores and the sociodemographic, clinical, and psychological variables analysed. Statistical tests utilized were Student’s t-test or ANOVA and the Mann-Whitney U test or Kruskal-Wallis test (tests were applied as appropriate, based on the normality of the variables analysed and the number of categories). Additionally, Spearman’s rho correlation coefficient was used to further investigate any significant relationship observed.
Using results from the univariate analysis, we developed general linear models for each dimension and components of the standardized scores of the SF-36. In all analyses, the independent variables included were all the sociodemographic, clinical and psychological variables that obtained a level of significance p < .05 in the univariate analyses.
Finally, mediation analyses were conducted to determine the mediating role of psychological variables between somatic symptoms and the physical and mental components of HRQoL. In these analyses PCS and MCS were taken as the dependent variables, the clinical variables (pain, fatigue and sleep disturbances) were included as the predictor variables and psychological variables (anxiety, depression, coping strategies and social support) were the mediating variables. The bootstrap method with 5000 resamplings was used to generate a bias correction with a 95% confidence interval for the indirect effect. The mediator variables were selected on assumptions required by the mediation analysis (independent variable as a predictor of the dependent variable; independent variable as a predictor of the mediator variable; and mediator variable as a predictor of the dependent variable). The mediator effect results were calculated using the formula: mediator effect = (1 – mediation proportion) × 100, in which the proportion mediation results from the formula: mediation proportion = direct effect/total effect (Hayes & Little, 2018).
The level of significance was set at p ≤ .05, and all analyses were conducted with the SPSS Version 24.0 statistical package.
Results
The study included a total of 134 patients (mean = 47.66 ± 9.99 years). Most of the sample were women (97%). Of the participants, 58 patients (43.3%) were selected in private rheumatology consultations, 16 (11.9%) in hospital rheumatology consultations, and 60 (44.8%) in hospital visits for chronic pain. The sociodemographic, lifestyle and clinical characteristics of the sample are presented in Table 1.
Table 1
Sociodemographic and clinical characteristics of the sample
The somatic and psychological characteristics of the sample are shown in Table 2. The findings indicate a high level of both physical and psychological symptoms among patients. In terms of anxious symptoms, high mean values were observed (13.66 ± 3.97), along with similarly high mean values for depression (11.34 ± 4.63). Scores for pain were also high, with a mean value in the MPQ of 47.15 ± 13.38, and for fatigue with a mean score in the FSS of 57.04 ± 8.47. Additionally, sleep disturbances were prominent, with a mean score in the PSQI of 12.85 ± 4.07.
Table 2
Somatic symptoms and psychological characteristics of the sample and internal consistency of the instruments used to assess these variables
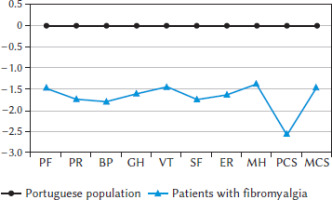
The sample of FM patients in this study had poorer HRQoL compared to the general Portuguese population of the same age. Using standardized scores of SF-36v2, the FM patients demonstrated lower scores in all dimensions and components, with magnitude above 0.80 indicating a large effect size according to Cohen’s classification (Cohen, 1988). The PCS indicated worse scores than the MCS (–2.56 ± 1.05 vs. –1.47 ± 1.03, respectively). The most affected dimensions were physical role functioning (–1.74 ± 0.98) and bodily pain (–1.81 ± 0.56), while the least affected dimension was mental health (–1.39 ± 1.20) (see Figure 1).
Figure 1
Standardized scores in the eight dimensions and two components of SF-36v2
Note. PF - physical functioning; PR - physical role functioning; BP - bodily pain; GH - general health; VT - vitality; SF - social functioning; ER - emotional role functioning; MH - mental health; PCS - physical component summary; MCS - mental component summary.
With the aim of identifying sociodemographic, clinical, and psychological factors associated with HRQoL, general linear models were conducted for each dimension of the SF-36, utilizing the stepwise method. In the models, candidate predictors included were sociodemographic, clinical and psychological variables that were identified by univariate analysis and the correlational analysis (data not shown). The results of the multivariable analyses of the SF-36 can be found in Table 3. The selected characteristics explained an acceptable proportion of variability (R2) in all dimensions and components (ranging from 16% for PCS to 54% for mental health). In 8 of 10 models analysed, the percentage of explained variance exceeded 25%, which is generally considered the minimum level above which the model can be deemed acceptable (Abraira & Pérez de Vargas, 1996).
Table 3
General linear model for SF-36v2 standardized scores
The multivariate analysis revealed that certain demographic and lifestyle variables were significant predictors of poorer HRQoL. Specifically, being non-active in terms of employment status was associated with poorer scores in physical role functioning and emotional role functioning (p ≤ .001), living in rural areas was associated with poorer scores in general health, vitality and PCS (p < .05), and having low educational levels was associated with poorer scores in mental health (p < .001).
Among clinical variables, longer duration of FM symptoms was associated with poorer scores in mental health (p < .01), having a psychiatric diagnosis was associated with poorer scores in physical functioning (p < .01), pain was associated with poorer scores in physical functioning, bodily pain, vitality, general health and PCS (p < .05), fatigue was associated with poorer scores in physical functioning, physical role functioning, PCS and MCS (p < .05) and experiencing sleep problems was associated with poorer scores in emotional role functioning (p < .01).
Regarding psychological variables, the presence of depression was consistently associated with worse HRQoL in multiple dimensions of the SF-36v2, including physical role functioning, general health, social functioning, emotional role functioning, mental health and in the MCS (p ≤ .05). The presence of anxious symptoms was also associated with worse HRQoL in several dimensions, including vitality, social functioning, mental health, and the MCS (p < .05). In addition, greater use of dysfunctional coping was associated with worse scores in mental health (p < .05), while social support was related to better scores in bodily pain, social functioning, emotional role functioning, and the MCS (p < .05).
The findings from the mediation analysis, which aimed to predict the SF-36v2 physical and mental components summary, are presented in Table 4 and Figure 2. The analysis included pain, fatigue, and sleep as independent variables, and anxiety, depression, coping, and social support as mediator variables. The psychological variables are not significant mediators in the relationship between pain and fatigue, and the physical area of SF-36v2 (insignificant indirect effects ranging from 6.6% to 7.4%). However, these variables do play an important role in the relationship between pain, fatigue, and sleep, and the mental area of HRQoL. Anxiety is a significant mediator in the relationships between pain (73.9%), fatigue (57.3%) and sleep (58.8%), and the MCS. Similarly, depression is a significant mediator between pain (84.7%), fatigue (29.5%) and sleep (51.5%), and the MCS. Dysfunctional coping is a significant mediator between pain (42.9%), fatigue (53.7%) and sleep (24.5%), and the MCS. Additionally, social support explains 49.8% of the relationship between fatigue and MCS, and 22.4% of the relationship between sleep disturbances and the MCS.
Table 4
Mediation analysis results for prediction of SF-36v2 physical and mental components summary
Discussion
The results of this study indicate that FM patients experience a negative impact on all dimensions of HRQoL, and the psychological variables play an important role as independent predictors of this decrease. Specifically, anxiety and dysfunctional coping primarily affect the mental dimensions of HRQoL, while depression and social support affect both physical and mental dimensions. Additionally, the psychological variables examined in this study mediate the effects of physical symptoms (pain, fatigue and sleep) on the mental domain of HRQoL, but not on the physical domain of HRQoL. It is important to highlight that these results refer mainly to women with FM, given the small number of men in the sample.
Compared to the general population of the same age group, patients with FM report a significant deterioration in HRQoL. This deterioration is evident across all domains and dimensions of HRQoL, although it is more pronounced in the physical domain than in the mental domain. PCS was more affected than MCS and the dimensions most affected by FM were physical role functioning and bodily pain (both of which correspond to the physical domain of HRQoL) and mental health was the least affected by FM. The profile of impaired HRQoL observed in this study, characterized by greater impairment in physical dimensions than in mental, is similar to what has been reported previously in the literature (Campos & Vázquez, 2012; Lee et al., 2017; Segura-Jiménez et al., 2015). However, it is important to note that the degree of HRQoL impairment found in this study is higher than what has been reported in some previous studies (Campos & Vázquez, 2012; Segura-Jiménez et al., 2015). This may be due to various reasons. Firstly, our sample was recruited from specialized healthcare services rather than patient associations, and patients in specialized healthcare services have a more severe clinical state (Häuser et al., 2011). Furthermore, a large proportion of our sample (44.8%) was recruited from tertiary healthcare facilities (chronic pain clinics). Recent studies have shown that this group of FM patients have higher impairment in their HRQoL compared to patients from secondary healthcare (Campos et al., 2021). Another possible explanation is that the majority of our patients (92.6%) were under 60 years old, which may also explain the observed HRQoL impairment, as young and middle-aged patients typically report a greater impact of FM on their HRQoL (Campos & Vázquez, 2013). Nonetheless, it should be noted that the FM-related impact on HRQoL observed in our study is not due to the presence of other concomitant rheumatic conditions, as this was controlled as an exclusion criterion. This is relevant since the presence of rheumatic comorbidity is very common in FM patients and can affect HRQoL (Jiao et al., 2016).
The data obtained in this study indicated that clinical and psychological variables are significant explanatory variables of HRQoL in FM patients. In contrast, sociodemographic variables had a limited effect, with only higher educational levels, living in urban areas, and being employed impacting a few SF-36 dimensions, which is consistent with previous studies (Ubago et al., 2008).
Among the clinical variables, pain was found to be one of the main explanatory variables of HRQoL, particularly in the physical dimensions (physical functioning, bodily pain, general health, vitality and PCS). Fatigue was associated with the physical domains (physical functioning, emotional role functioning, and PCS) as well as the MCS. These findings are consistent with previous studies (Campos & Vázquez, 2012; Oncu et al., 2013). Although sleep disturbances are prevalent in FM patients (Wu et al., 2017), after controlling for sociodemographic, clinical and psychological variables, they were only found to be related to emotional role functioning. Sleep problems have been associated with negative affect (Kishi et al., 2010), which could lead to interference with daily activities due to emotional issues.
Regarding psychological variables, after controlling for various sociodemographic and clinical variables, our findings indicate that depression is significantly associated with decreased functioning in multiple domains, including physical role functioning, general health, social functioning, emotional role functioning, mental health, and MCS. On the other hand, anxiety is linked to lower scores in the SF-36 mental area (vitality, social functioning, mental health, and MCS). These results underscore the critical role of depression and anxiety in the HRQoL of patients with FM. The high prevalence of anxiety (81.3%) and depression symptoms (56%) highlights the need to take into account these psychological variables in evaluating and enhancing HRQoL in FM patients.
The association of the somatic symptoms of FM with psychological symptoms and disorders has led some specialists to classify FM as a somatic symptom disorder according to the classification of the fifth version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). However, other specialists propose a biopsychosocial model of FM that emphasizes the neurological underpinnings of this disease and attributes importance to psychosocial factors in the predisposition, triggering and chronification of symptoms (Hauser & Fitzcharles, 2018). In any case, the accumulated evidence underlines the importance of considering and treating psychiatric disorders and psychological factors that affect pain management (Sancassiani et al., 2017).
In this study neither problem-focused coping nor emotion-focused coping was associated with worse HRQoL in FM patients, indicating that both coping strategies could be adaptive. However, dysfunctional coping was related to a greater impact on the mental health dimension, possibly due to the association between dysfunctional coping and emotional distress (McInnis et al., 2014).
Our results are consistent with previous research studies indicating that individuals with FM experience low levels of perceived social support (Gündüz et al., 2019; Montoya et al., 2004). The unpredictable and intense symptoms associated with FM often make it challenging for patients to plan social activities with their family, friends, or partners. Moreover, as FM symptoms are not visible and cannot be detected by any abnormal tests, it may lead social supporters to assume that the patient is simulating their illness, resulting in reduced social support. This lack of social support may also increase the potential stigmatization of patients, which further exacerbates the negative impact of FM on patients’ social life (Asbring & Narvanen, 2002). Our study found a significant association between good social support and better mental dimensions such as social functioning, emotional role functioning, and MCS, as well as lower levels of bodily pain. These results are in line with some previous research studies in FM patients (Gündüz et al., 2019; Montoya et al., 2004) highlighting the crucial role of social support in improving both the mental and physical dimensions of HRQoL, and also consistent with the recent study by Schetsche et al. (2023) in the general population which revealed that levels of social support have significant effects on psychological symptoms. Our findings emphasize that social support can be an essential resource that enhances HRQoL, underscoring the importance of providing adequate social support to patients with FM, and shows the importance of social support as a beneficial resource in HRQoL.
Taken together, these findings suggest that clinical variables (primarily pain and fatigue) are more closely associated with the physical domain of HRQoL, whereas all psychological variables are more closely associated with the mental domain of HRQoL, and depression and social support are also associated with some physical dimensions.
In addition to the direct influence of anxiety, depression, dysfunctional coping and low social support on HRQoL, this study showed a secondary influence of these variables via mediating the negative influence of clinical variables (pain, fatigue and sleep disturbances) on the mental domain of HRQoL, but not the physical domain. These findings suggest that somatic symptoms (such as pain, fatigue and sleep problems) may trigger feelings of depression and anxiety and dysfunctional coping mechanisms among FM patients, indirectly increasing the negative impact of these somatic symptoms on MCS. The limitations imposed by fatigue and sleep problems can restrict social activities and lead to isolation, resulting in decreased social support, which has been linked to a decrease in the mental dimension of HRQoL. To the best of our knowledge, this is the first study to show that anxiety, depression, coping and social support also play a mediating role between the symptoms of fatigue and sleep problems and the mental domain of HRQoL.
Contrary to the results of Gálvez-Sánchez et al. (2020a, b), no mediating influence of anxiety, depression or coping strategies was observed on the relationship between pain and the physical dimensions of HRQoL. Due to the limited literature on this aspect, it is challenging to establish the reasons for these discrepancies. A possible explanatory hypothesis could be that in patients with a lower level of severity (as seen in the samples from Gálvez-Sánchez’s studies) the impact of somatic symptoms on the physical dimensions of HRQoL is mediated by psychological variables. However, this may not happen in more severe patients (as in the case of the present sample). In our study we also did not find that the psychological variables anxiety, depression, dysfunctional coping and social support mediate the relationships between other physical symptoms (fatigue and sleep problems) and the physical domain of HRQoL. The mediating role of psychological variables in the effect of physical symptoms of FM on physical domains of HRQoL should be further explored in future research.
Among strengths of this study, it is worth noting the inclusion of a wide range of sociodemographic, lifestyle, anthropomorphic, clinical, and psychological variables, thus providing a clearer picture of the predictors of HRQoL. Additionally, the study sample consisted of FM patients without any other rheumatic conditions, which are prevalent comorbidities that can confound the specific effects of FM on HRQoL. Moreover, data collection was conducted across multiple centres, which enhances the generalizability of the findings. Finally, the mediational analyses provide better insights into the complex interrelation among predictors. Overall, these strengths contribute to a robust understanding of the factors influencing HRQoL in FM patients.
This research also has some limitations. Firstly, despite the inclusion of a wide range of measures, variables such as the type of pharmacological treatment or psychological variables such as self-esteem or self-efficacy were not taken into consideration. Furthermore, although the sample showed a similar sex distribution as that observed in the Portuguese FM population, the predominantly female sample limits the generalizability of the findings to men.
Conclusions
In conclusion, this study highlights the significant negative impact of FM on patients’ HRQoL across physical, emotional, and social dimensions. Both clinical variables (pain, fatigue and sleep disturbances) and psychological variables (anxiety, depression, dysfunctional coping, and low social support) have a direct effect on HRQoL of FM patients. Furthermore, psychological variables may indirectly increase the negative influence of clinical symptoms on the mental dimension of HRQoL. These findings underscore the importance of assessing and treating psychological variables as part of multidisciplinary therapeutic programmes incorporating interventions to reduce anxiety and depression, decrease the use of dysfunctional coping strategies and increase social support. Future research could explore the role of psychological variables as an indirect mechanism in the association between pain, fatigue and sleep disorder and physical domains of HRQoL in FM patients.



