BACKGROUND
SUICIDE IN JAPAN
Suicide is a serious public health problem around the world. According to the World Health Organization (WHO), annually, approximately 800,000 people commit suicide worldwide. Suicide is also the second leading cause of death among 15-29-year-olds and the fifth leading cause of death among 30-49-year-olds worldwide (WHO, 2019b). Furthermore, suicide imposes a significant socioeconomic burden on families, communities, and nations (WHO, 2019a).
Suicide rates are high in Japan, with suicide being one of the top ten causes of death (Nomura et al., 2017), especially among working-age men (Wada & Gilmour, 2016). Despite Japan’s suicide rate decreasing over recent years (Dhungel et al., 2019), data from the Organization for Economic Cooperation and Development (OECD) reported that Japan’s suicide rate was still the sixth-highest among member countries as of 2017 (OECD, 2018). In 2018, the number of suicides was 20,840, which is a suicide rate of 16.5 per 100,000 (Ministry of Health, Labour and Welfare, 2018). Among the risks associated with suicide, suicidal ideation (SI) is a strong predictor of death by suicide (Nock et al., 2008; WHO, 2019b). The identification of individuals at high risk of attempted suicide and provision of follow-up care and support are essential components of a comprehensive suicide prevention strategy.
THE ASSOCIATION BETWEEN INSOMNIA AND SUICIDAL IDEATION
Insomnia is not only associated with poor physical and mental quality of life, reduced work productivity, and impaired activity (Bolge et al., 2009), but it is also associated with a risk for independent SI (McCall & Black, 2013; Pigeon et al., 2014). Recently, several studies have examined the association between sleep status and SI (Kim et al., 2013; Owusu et al., 2020). Japan has the highest rate of insomnia complaints and the shortest average sleep duration among the OECD countries (OECD, 2020), with the working-age population being the most prone to sleep deprivation and insomnia. The National Health and Nutrition Survey conducted by the Ministry of Health, Labour and Welfare (MHLW) in 2017 surveyed men and women over 20 years of age to determine the average daily hours of sleep (based on the past month). The results showed that 30.9% of respondents in their 40s said they were not getting enough rest or not sleeping at all, while 28.4% of respondents in their 20s said they were not getting enough sleep (Ministry of Health, Labour, and Welfare, 2017).
SENSE OF COHERENCE (SOC)
Salutogenesis, a theory put forward by Aaron Antonovsky, is an approach to medicine that aims to investigate factors that support health and the “origin of health” rather than focusing on disease and pathogenesis (Antonovsky, 1979, pp. 1–3, 1985, p. 278). Within this theory, sense of coherence (SOC) is an important concept that encompasses three elements: comprehensibility, manageability, and meaningfulness. SOC is the ability to cope successfully with psychological stress and thereby maintain and improve health (Antonovsky, 1985, p. 275). Differences in SOC are observed between individuals and, in particular, those with low SOC are reported to have more SI/suicide attempts (Giotakos, 2003; Mehlum, 1998). Meanwhile, it has been reported that high SOC can alleviate suicidal ideation associated with high psychological stress (Drum et al., 2016). Taken together, the findings of these studies suggest that there are characteristics of SI associated with SOC level.
Traditional multivariate analyses are done with the assumption that each sample is independent; however, if the analysis ignores the high degree of within-population similarity in the actual data it can lead to the Type I error in which the standard error is estimated to be small (Harrison et al., 2018). For analyses that consider within-group similarity, multi-level analyses that factor in differences between groups as a variable effect are appropriate. For example, some reports have examined the presence or absence of SI at the individual level for level 1 (fixed effects) and the city level for level 2 (random effects) (Tan et al., 2016). However, to the best of our knowledge, there are no reports examining the insomnia/SI association with SOC as a random effect.
Therefore, in the present study, we conducted a multi-model analysis of the association between insomnia and SI among Japanese workers with SOC as a random effect to examine whether populations with low to high SOC show an association between insomnia and SI.
PARTICIPANTS AND PROCEDURE
RESEARCH DESIGN AND PARTICIPANTS
We conducted a cross-sectional survey using data from the Tsukuba Science City Network (TSCN), which is an organization whose purpose is to promote inter-institutional collaboration within Tsukuba Science City’s research and academic institutions. This large-scale cross-sectional survey, called the 7th Life Environment and Workplace Stress Survey, was carried out among workers in Tsukuba Science City. The study, which was initiated in 1986, was conducted by the Special Committee on Mental Health Measures at the TSCN (Sato, 1991) in response to the emergence of a perceived suicide-inducing condition known as the “Tsukuba syndrome” that gained notoriety in the 1970s and gained national attention in the early 1980s due to an alleged high incidence of suicide among researchers (Hamilton, 1992). Oda (1991) posited that the relocation of the institute to Tsukuba City in 1970s rendered the staff more susceptible to depression due to the spatial distance between their residences and workplaces, which necessitated a reliance on vehicular transportation, and a lack of social interaction among residents. The present study, conducted in 2017, represents the seventh iteration of this ongoing research series. As of 2017, the TSCN comprised 89 organizations from research institutions, universities, educational foundations, municipalities, and private companies throughout the city. A total of 19,481 workers from 53 organizations, mostly research and educational institutions, agreed to participate. The number of respondents was 7,255, which is a response rate of 37.2%. The analysis included 7,175 participants between the ages of 20 and 65, as Japan’s official retirement age is 65. The data collection method is described in detail elsewhere (Hori et al., 2019).
MEASURES
Suicidal ideation. SI was investigated using the same methodology as described in the study by Hori et al. (2019). Questions regarding SI were asked in two steps. First, the respondents were asked, “Have you ever seriously thought of committing suicide” with the answering options of yes, no, and no response. Second, respondents who answered “yes” proceeded to the next question, “Have you thought of committing suicide in the past year?” with the same answering options as the first question. Respondents who answered “yes” to both the first and second questions were categorized as having SI in the past year. Respondents who gave no response at all or who answered “no response” to either the first or second questions were excluded from the analyses. The remaining respondents were categorized as being without SI in the past year.
Athens Insomnia Scale (AIS). The Athens Insomnia Scale (AIS) was developed based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) by the World Health Organization (Soldatos et al., 2000). The AIS consists of eight items; the first five pertain to sleep induction, awakenings during the night, final awakening, total sleep duration and sleep quality, while the last three refer to well-being, functioning capacity, and sleepiness during the day. All items were rated using a 4-point Likert scale from 0 (no problem) to 3 (a severe problem), and a cut-off score of 6 was used to indicate insomnia (Soldatos et al., 2000).
The Japanese version of the AIS was used in this study (Okajima et al., 2013). Cronbach’s α for the AIS in this study was .83.
The five-point SOC-13 scale. The Japanese version of the 13-item five-point SOC scale was used in this study with permission from the copyright holder (Antonovsky, 1987; Antonovsky et al., 1985; Togari & Yamazaki, 2005). The five-point-13-item SOC scale corresponds to the three components of SOC: five items related to comprehensibility, four items related to the sense of manageability, and four items related to meaningfulness. Responses are given on a five-point Likert scale, with higher total scores indicating stronger SOC (range from 13 to 65). The mean and standard deviation (SD) of the scores were calculated. Scores less than –1 SD were classified as the low group, +1 SD or more as the high group, and the remaining scores as the medium group. Cronbach’s α for the 13-item five-point SOC scale in this study was .86.
Kessler Screening Scale (K6) for psychological distress. The Japanese version of the K6 was used in this study (Furukawa et al., 2008). The K6 measures the frequency of experiencing six different symptoms of psychological distress over the preceding 30 days: (1) nervousness, (2) hopelessness, (3) restlessness, (4) depression, (5) worthlessness, and (6) everything was an effort. Each item is rated on a 5-point scale, ranging from 0 (none of the time) to 4 (all of the time). Responses were summed to create a composite score (range 0 to 24) with a score of 13 or higher suggesting serious mental illness (Furukawa et al., 2008). Cronbach’s α for the K6 in this study was .90.
Other covariates. Participants were categorized into the following four age groups: 20-29, 30-39, 40-49, and 50-65 years. Smoking habits, exercise habits, and current hospital attendance were investigated. Participants’ annual household income (Japanese yen) was classified into four groups: < 4 million, 4-8 million, 8-12 million, and ≥ 12 million. Occupation was derived from the item: “Which of the following best describes your job?” with the answer options of “researcher/academic,” “technician/engineer,” and “clerk/administration” and “others.” Participant’s marital status was classified as: “married,” “single,” “divorced,” and “bereavement (separated by death)”. Participant’s educational level was categorized as: “high school,” “college, national institute of technology, or vocational school,” “undergraduate,” and “graduate school.” Participants were also asked about whether they were currently attending hospital including clinics, dental clinics, masseuse, acupuncture, and judo therapy.
STATISTICAL ANALYSIS
Chi-square tests were used for categorical independent variables to compare the characteristics of those who had a history of SI in the past year with those who did not. Next, logistic regression curves for each SOC group were created to examine whether there were differences in the distribution of insomnia (AIS ≥ 6) and SI in each SOC group. A model without any predictors was run to examine whether a multi-level logistic model should be implemented and compute the intraclass correlation coefficient (ICC). ICC can be calculated as follows (Sommet & Morselli, 2017):
In this study, two statistical models were constructed. The first model was a binomial logistic multi-model analysis with SI as the dependent variable and insomnia (AIS ≥ 6) as the independent variable (Model 1). The second model was a binomial logistic multi-model analysis with each of the AIS sub-items as independent variables (Model 2). Both models were adjusted for the association between insomnia and SI by controlling for socioeconomic factors (age, sex, education level, household income, marital status) and health behaviours (smoking status, exercise habits), as well as further adjusting for health status (current hospital attendance; psychological stress, K6 ≥ 13). The goodness of fit of the models was evaluated by calculating the area under the receiver operating characteristic curve (AUC).
R version 4.03 was used for the statistical analyses and ggplot2 package version 3.3.2 (Wickham, 2016) was used to draw the graphs, and lme4 package version 1.1-23 (Bates et al., 2015) was used for multi-level analysis.
RESULTS
DESCRIPTIVE FEATURES
Among those surveyed, 752 were excluded from the analysis due to non-response or invalid responses. Finally, 6,423 were included in the analysis. Among those, 418 individuals had SI in the past year, and 6,005 had no SI in the past year. Table 1 shows the study population’s demographic characteristics by the presence or absence of SI in the past year.
Table 1
Demographic characteristics
Insomnia (AIS ≥ 6) was statistically significantly higher in the group with SI (n = 312, 74.6%) than in the group without SI (n = 2,278, 37.9%) (χ2 test p < .001).
DISTRIBUTION OF INSOMNIA AND SI BY SOC GROUP
The mean and SD of the SOC-13 score was 57.30 and 12.70, respectively. The SOC scores were classified into three groups: low: 13-44 (n = 908), medium: 45-69 (n = 4,377), and high: 70-91 (n = 1,138). Logistic regression curves were created by plotting the distribution of AIS scores and SI for each SOC group (Figure 1). The intercept of the logistic curves was different in the low and medium SOC groups, and the slope of the curves was different in the high SOC group, indicating an interaction between SI and SOC in the high SOC group. Analyses showed an interaction between AIS scores and the SOC high group (odds ratio [OR] = 0.16, 95% CI [0.07, 0.37], p < .001).
Figure 1
Logistic regression curves and distribution of AIS scores and suicidal ideation for each SOC group
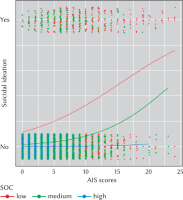
Table 2 presents results showing the number of participants with insomnia and SI per SOC group; in the high SOC group, only one participant with SI was found to have insomnia and SI (Fisher’s exact test p = 1.00).
Table 2
Insomnia and suicidal ideation in the past year by SOC groups
MULTI-LEVEL BINOMIAL LOGISTIC REGRESSION ANALYSIS
Because there was only one participant with SI in the high SOC group, we excluded this group from the analysis and conducted a multi-level analysis using a random slope model with the low and middle SOC groups (n = 5,285) as random effects.
Table 3 shows the results of the analysis with SI as the dependent variable in Model 1. The ICC was 0.11; that is, the variation between SOC groups accounted for 11% of the variance in the presence or absence of SI. The variance inflation factor (VIF) was higher than 10 for the occupational variables and was determined to be multicollinear and was excluded from the covariates. The odds ratio (95% CI) for insomnia (AIS ≥ 6) after adjusting for covariates was 2.26 (95% CI [1.75, 2.93]).
Table 3
Multilevel logistic regression analysis
Table 4 presents the results of the analysis with SI as the dependent variable in Model 2. The ICC was 0.895, indicating that 8.95% of the variance in the presence or absence of SI was accounted for by variation between SOC groups. Similar to Model 1, the VIF for the occupational variables was higher than 10, indicating multicollinearity, and thus they were excluded from the covariates. Among the AIS sub-items, “Final awakening earlier than desired” (OR = 1.26, 95% CI [1.05, 1.50]) and “Sense of well-being during the day” (OR = 1.63, 95% CI [1.34, 1.99]) were found to be associated with SI. The AUC for Model 1 was 0.83 (95% CI [0.81, 0.85]) and for Model 2 it was 0.84 (95% CI [0.82, 0.86]).
Table 4
Multilevel logistic regression analysis
DISCUSSION
SI AND RELATED FACTORS
The results of the present study indicate that insomnia is associated with SI over the past year among AIS-indexed workers; this is the first multi-level analysis to use SOC as a random effect.
Even after adjusting for socioeconomic and health factors, insomnia was associated with SI. These results are consistent with previous studies (McCall & Black, 2013; Pigeon et al., 2014). In our analysis of the AIS sub-items, we found that the sub-items “Final awakening earlier than desired” and “Sense of well-being during the day” were associated with SI. “Final awakening earlier than desired” describes a condition in which an individual wakes up during the night or early in the morning and is unable to return to sleep. Our results align with previous studies on sleep status, as it has been reported that night-time wakefulness is associated with SI (Tubbs et al., 2020, 2021). Additionally, our findings are consistent with previous research that has established a link between psychological well-being and SI (Jin & Zhang, 1998).
Our multilevel analysis also revealed that insomnia was associated with SI, with variation between SOC groups potentially accounting for 11% (Model 1) and 8.95% (Model 2) of the variation in the presence or absence of SI. Interestingly, there was an interaction with AIS scores in the high SOC group. Furthermore, only one participant in the high SOC group developed SI, and he did not have insomnia. Hence, the findings suggest that high SOC has a mitigating effect on SI.
There is no conclusive evidence on the mechanism behind the association between insomnia and SI, but several psychological and biological hypotheses have been proposed (McCall & Black, 2013). For example, the psychological hypothesis proposes a model in which dysfunctional beliefs and attitudes about sleep, feelings of hopelessness, and nightmares influence SI. Given our results, high SOC may buffer SI by suppressing perceptions of dysfunctional beliefs and attitudes about sleep, feelings of hopelessness, and nightmares. One possible mechanism is that the comprehensibility, manageability, and meaningfulness observed with high SOC may influence insomnia perception. It has also been reported that higher SOC is associated with less despair (Petrie & Brook, 1992). The association between SOC and nightmares is unclear and should be examined in the future. Because the SOC questionnaire indicated no reliable replication of the sub-items’ comprehensibility, manageability, and meaningfulness (Antonovsky, 1993), and other measures should be used to examine which of the three SOC sub-items are at work in SI.
The distribution of SOC in the present study was almost identical to SOC’s distribution in the Japanese population in a previous study (Togari et al., 2015) and did not deviate significantly from the general population. Because Togari and colleagues (2015) included participants of up to 75 years of age, the likely mean of the SOC is somewhat higher than in our study, because SOC tends to be higher in older age groups (Feldt et al., 2010, 2006; Koelen et al., 2017).
For covariates, current smokers, lower exercise habits, and current hospital visits were associated with SI. These results are consistent with previous studies (Ahmedani et al., 2017; Davidson et al., 2013; Fukai et al., 2020; Poorolajal & Darvishi, 2016). High psychological stress (K6 ≥ 13), suggesting nonspecific serious mental illness, was also associated with SI.
Workers in their 20s were more likely to have SI than workers of other ages. Perhaps younger workers are more susceptible to psychological stress than middle-aged workers. Younger people tend to work longer hours and experience greater mental stress. Working long hours is a risk factor for mental illness and suicide (Park et al., 2020). Because this study did not survey working hours, a detailed survey of working hours for each age group is needed in the future. Associations between women, low education and low-income levels and SI have been reported (Bantjes et al., 2016; Phillips & Hempstead, 2017; Yoshimatsu et al., 2006), but such associations were not evident in this study.
IMPLICATIONS AND SUPPORT FOR PEOPLE WITH SUICIDAL IDEATION
Insomnia is a risk factor for SI and a risk for suicide with an even higher fatality rate (Pompili et al., 2013), and the detection and intervention of patients who complain of insomnia are necessary. Recently, a study demonstrated the efficacy of extended-release zolpidem tartrate in reducing symptoms of insomnia associated with depression (McCall et al., 2019). However, there is a scarcity of research on alternative interventions for reducing symptoms of insomnia. Additionally, it is crucial to note that zolpidem has been documented to have properties of abuse and dependence; thus its prescription should be approached with caution and in accordance with appropriate medication management protocols (Victorri-Vigneau et al., 2007).
According to Antonovsky, SOC develops throughout a persons’ formative years until early adulthood, up to their 30s. However, it has been shown that SOC can grow beyond early adulthood (Feldt et al., 2006, 2010; Koelen et al., 2017). Our results suggest that increasing the level of SOC may help to reduce the SI that results from insomnia. According to research by Super et al. (2016), there are two approaches to enhancing SOC. The first process is a behavioural approach that enables people to identify appropriate generalized resistance resources (GRRs), which refers to the different resources a person mobilizes when dealing with stressors in their daily life as a coping mechanism. The second process is to reaffirm the stressful situation a person is facing, which is a cognitive approach to understanding stressors and identifying the GRRs to help them identify and feel meaningful when dealing with those stressors.
In clinical practice, the effectiveness of the Resource Enhancement and Activation Program (REAP) self-care program has been reported (Khoon Kiat et al., 2014). This program targets older adults and encourages them to activate their personal and community resources. It is expected that effective SOC improvement programs for all age groups will be developed in the future.
Employer-led interventions to improve employees’ sleep are also needed. Long working hours have been reported to be a risk for short sleep and insomnia (Virtanen et al., 2009); thus, ensuring adequate sleep and addressing the issue of long working hours is vital. Redeker and colleagues reviewed the literature on interventions that employers could initiate to improve employees’ sleep (Redeker et al., 2019). They included health promotion interventions such as educational programs for day and shift workers, promotion of physical activity, strategic napping, and improvement of the work environment, all of which showed promising findings. Future research is needed to determine whether improving workers’ sleep leads to physical and mental health improvements.
LIMITATIONS
This study has the following limitations. Firstly, there is a potential for false negatives in the assessment of symptoms of SI and insomnia in the high SOC group. Secondly, the low response rate of 37.2% for this survey may have resulted in a response bias. Thirdly, we were unable to control for potential confounders such as major depressive disorder (MDD), which is associated with both insomnia and SI (Cai et al., 2021). Although we adjusted our statistical model by using a history of current hospital visits as a proxy for assessing pre-existing conditions and psychiatric disorders, as well as severe psychological stress as defined by K6 ≥ 13, we were unable to examine specific diagnoses. As a result, it is plausible that some of the participants in this study may have insomnia secondary to a mental illness. The treatment of SI in such individuals necessitates addressing both the underlying disease and sleep problems. Furthermore, we did not adjust for other potential confounders such as alcohol abuse (Sung et al., 2015), working hours (Park et al., 2020; Yoon et al., 2015), and social capital (Hori et al., 2019). Fourthly, the causal relationship between the variables is unknown as the current study is cross-sectional in design. MDD has been reported to be associated with pessimistic and negative cognitions (Gotlib & Joormann, 2010), and it is possible that such cognitions may negatively affect SOC. Future research is needed to examine MDD in this population and follow-up studies are required. In addition, the study used a self-reported questionnaire, the AIS, to investigate insomnia, and self-report measures are known to have recall bias. For instance, self-reported sleep duration may overestimate objective sleep measures such as polysomnography and actigraphy (Jackson et al., 2018). Furthermore, this study does not adequately differentiate between insomnia and sleep deprivation. Sleep deprivation is a disorder distinct from insomnia, but as it is associated with daytime sleepiness and reduced daytime activity (Chattu et al., 2018), it is possible that those with sleep deprivation may also be determined to have insomnia by the AIS. Therefore, it is possible that some individuals determined to have insomnia by the AIS may in fact have sleep deprivation syndrome. Detailed sleep assessment requires the use of sleep diaries and actigraphy. As Japan has a higher percentage of workers working long hours than other countries (Okamoto, 2019), sleep deprivation syndrome may be more prevalent and may be associated with SI. Additionally, it may be more appropriate to measure SI using a validated scale such as the Columbia Suicide Severity Rating Scale (C-SSRS; Posner et al., 2011).


