BACKGROUND
Psycho-oncological care (PC) supports cancer patients in coping with and minimising psychological and social problems in the context of their disease (Mehnert, 2014; Weis et al., 2007). It focuses on enabling patients to develop and adapt coping strategies to minimise psychological distress while increasing quality of life and strengthening social resources (Graves, 2003; Osborn et al., 2006; Schumacher, 2004; Weis et al., 2007). A psycho-oncological treatment approach is usually patient-centred, characterised as resource- and problem-oriented (Leitlinienprogramm Onkologie, 2014; Sperner-Unterweger, 2011; Weis et al., 2007). Salutogenesis, a concept shaped by the medical sociologist Antonovsky, focuses on resources of various kinds (e.g. individual, group/community and organisational) that help a person to cope with life stressors and promote their health (Antonovsky, 1987). Hence, PC facilitates a salutogenic way for patients to cope with their illness and mentally stabilise. This study aimed to assess whether PC affects patients’ salutogenesis. For this, it is important to understand why the working relationship (therapeutic alliance) between the psycho-oncologist and patient as well as a salutogenic outcome is imperative in cancer care.
THE THEORY OF SALUTOGENESIS
The theory of salutogenesis focuses on the interactions between stressors and health-promoting (salutary) factors and how they lead to a healthier movement on the ‘health ease/dis-ease continuum’ (Antonovsky, 1987; Vinje et al., 2022). Salutogenesis integrates a person’s complex history and abilities to adapt to a potentially stressful life experience (Antonovsky, 1987). Figure 1 illustrates a simplified version of the core components of the theory of salutogenesis.
Figure 1
A simplified illustration of the theory of salutogenesis (Antonovsky, 1987) focused on key concepts
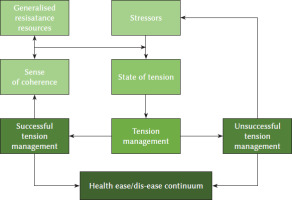
Generalised resistance resources encompass characteristics of a person or group/community which provide life experiences that are consistent and balanced and lead to greater participation in decision-making (Antonovsky, 1987; Idan et al., 2017). These resources can be diverse and individual (e.g. material resources, knowledge or social support) based on a person’s social, cultural and historical context (Antonovsky, 1987). At the same time, stressors exist in a person’s life (Antonovsky, 1987), which may lead to a state of tension that looks different depending on the stressor. How a life stressor is managed depends on one’s generalised resistance resources and the so-called ‘sense of coherence’ (SoC) (Antonovsky, 1987). The SoC stands for an orientation in life towards successfully coping with life events, thereby maintaining and promoting health (Antonovsky, 1987). Generalised resistance resources have a decisive influence on SoC’s development, which consists of three components: comprehensibility, manageability and meaningfulness. SoC is defined as follows:
The sense of coherence is a global orientation that expresses the extent to which one has a pervasive, enduring though dynamic feeling of confidence that (1) the stimuli deriving from one’s internal and external environments in the course of living are structured, predictable, and explicable; (2) the resources are available to one to meet the demands posed by these stimuli; and (3) these demands are challenges, worthy of investment and engagement (Antonovsky, 1987, p. 19).
The theory of salutogenesis states that the SoC enables a person to choose the most appropriate coping strategy for a respective life stressor, thus promoting health (Antonovsky, 1987). Hence, the SoC mobilises generalised resistance resources to interact with a person’s state of tension, manage a holding action and overcome the stressor (Antonovsky, 1987). Tension management can have different outcomes: 1) successful tension management that can strengthen the SoC and positively regulate a person’s place on the health ease/dis-ease continuum versus 2) unsuccessful tension management that can lead to a state of stress that negatively affects a person’s place on the health ease/dis-ease continuum (Antonovsky, 1987).
SENSE OF COHERENCE IN CANCER PATIENTS
Antonovsky (1987) suggested that a strong SoC increases the acceptance of a disease and treatment while improving functioning during the disease. Numerous studies have indicated a relationship between the SoC, quality of life and self-assessed health status of cancer patients (Eriksson & Lindström, 2007; Gerasimčik-Pulko et al., 2009; Kenne Sarenmalm et al., 2013; Lindblad et al., 2018; Rohani et al., 2015a). A high SoC positively associates with better quality of life after treatment (Kenne Sarenmalm et al., 2013; Rohani et al., 2015b; Shapiro et al., 2001), reduced levels of symptom burden (Kenne Sarenmalm et al., 2014) and better mental well-being after surgery or during chemotherapy (Black & White, 2005; Boman et al., 1999; Hiensch et al., 2020). In contrast, a low SoC is associated with more distress, worse quality of life and a health status independent of the disease stage or treatment (Kenne Sarenmalm et al., 2013). Furthermore, age, gender, ethnicity, disease stage and time since diagnosis have been found to be non-significant moderators in the association between the SoC and the level of distress (Winger et al., 2016) as suggested by Antonovsky (1987). SoC mediates the global quality of life and cognitive and social functioning within a period of six months and partially mediates changes in emotional functioning, well-being, mental health, fatigue and financial difficulties (Rohani et al., 2015a, b). Therefore, SoC acts as a significant mediator in other patient-reported outcomes.
Improving patients’ SoC in healthcare settings may be implemented differently. For example, patients should receive understandable health information to promote comprehensibility, especially considering their health literacy levels (Pelikan, 2017; Sørensen et al., 2015). Increasing manageability can mean enabling patients to care for their conditions while, if needed, offering specific support to promote self-management, such as case management or psychosocial care (Pelikan, 2017). Meaningfulness may be promoted by person-to-person interaction, such as psychological support that helps patients make sense of their situations (Pelikan, 2017) against the background of their life experiences and values (Diegelmann, 2016). Consequently, it is unsurprising that SoC positively relates to patient satisfaction with health services (Larsson et al., 1999; Tistad et al., 2012).
Research has sought to apply the salutogenesis model to predict tension and tension management in the context of PC. The results have shown that generalised resistance resources and SoC partially predict the need for PC (tension; Cecon et al., 2021). SoC and generalised resistance resources have functioned as salutary factors, whereas the absence of generalised resistance resources more likely resulted in the need for psycho-oncological care. Moreover, PC utilisation (tension management) was partially predicted by the need for care, generalised resistance resources and SoC. Lower SoC made it more likely to develop a need for PC and to utilise care. These results aligned with the conceptual basis of Antonovsky’s model of salutogenesis. However, if and how the utilisation of PC (tension management) affected patients’ salutogenic path on the health ease/ dis-ease continuum could not be assessed due to data availability restrictions (Cecon et al., 2021).
THERAPEUTIC ALLIANCE
Therapeutic alliance reflects the quality of the emotional bond and collaborative relationship between a therapist and patient in the context of psychotherapy (Bordin, 1979; Flückiger et al., 2018; Horvath & Symonds, 1991; Mack et al., 2009; Orlinski et al., 1994; Wilmers et al., 2008). This alliance is characterised by the ability of the therapist and patient to form a personal bond that develops trustworthiness and a feeling of security (Horvath & Symonds, 1991; Martin et al., 2000). Various studies have shown therapeutic alliance to be a reliable predictor of treatment success across different patient populations and therapeutic modalities (Crits-Christoph, 1999; Horvath et al., 2011; Horvath & Symonds, 1991; Malin & Pos, 2015; Martin et al., 2000; Norcross & Lambert, 2011; Sammet et al., 2004; Vitinius et al., 2018; Waddington, 2002). Similar results have been obtained in the therapeutic care of cancer patients, where a handful of studies have shown successful therapy outcomes influenced by a good therapeutic alliance (Applebaum et al., 2012; Katz et al., 1987; Leuteritz et al., 2017; Manne et al., 2010; Zwerenz et al., 2012).
However, empirical studies on the effect of therapeutic alliance in PC with cancer patients have been rare overall (Leuteritz et al., 2017), although patients have highlighted the importance of a good relationship with their psychotherapist (Nissim et al., 2012). Studies and meta-analyses on psychotherapeutically treated non-cancer patients have suggested that therapeutic alliance is a critical influencing factor for patient satisfaction since it improves the quality of care and facilitates positive treatment outcomes (Bar-Sela et al., 2016; Flückiger et al., 2018; Leuteritz et al., 2017; Marmarosh & Kivlighan, 2012; Nienhuis et al., 2018; Rehse & Pukrop, 2003; Rozmarin et al., 2008). Similar results were obtained in the evaluation of a new complex psycho-oncological intervention programme, which indicated that therapeutic alliance positively affected cancer patients’ satisfaction with their PC, with patients assessing it as more needs-oriented (Krieger et al., 2022).
OBJECTIVE
The theory of salutogenesis is a valuable guiding model for research focused on strengthening health outcomes. However, more research is needed to understand how SoC can be strengthened (Hochwälder, 2022; Suominen & Lindstrom, 2008). In the context of PC, we aim to contribute to this agenda by evaluating the components of tension management and SoC. Based on the literature and the theory of salutogenesis, we define the cancer diagnosis as a life stressor that possibly creates tension. PC may be a way to manage this tension. More precisely, building a strong therapeutic alliance with the psycho-oncologist may facilitate the care process and positively influence the state of tension and successful tension management. According to the salutogenesis model, successful tension management may strengthen patients’ SoC and positively affect their positions on the health ease/dis-ease continuum (Antonovsky, 1987). Hence, we aim to empirically assess whether the relationship between cancer patients and their psycho-oncologists (therapeutic alliance) positively influences patients’ salutogenesis process by facilitating needs-oriented care. Here, we hypothesise that contact with a psycho-oncologist (needs-oriented utilisation of consultations) and therapeutic alliance built during these contacts positively influence patients’ SoC over time.
PARTICIPANTS AND PROCEDURE
CARE SETTING AND DATA COLLECTION
We used external evaluation data from the project ‘isPO’ (integrated cross-sectoral psycho-oncology) for our research question. The project sought to develop, implement and evaluate a new complex psycho-oncological form of care to reduce anxiety and depression in newly diagnosed cancer patients based on individual needs during a 12-month period (Jenniches et al., 2020; Kusch et al., 2022). In 2019, a new form of care (nfc), isPO, was implemented in four newly established PC networks in North-Rhine Westphalia, Germany. They consisted of cooperation between certified oncological cancer centre hospitals and local oncological practices. Within the care networks, various professionals provided PC, including physicians (e.g. oncologists) as referrers, licensed psychotherapists, psychosocial professionals and case managers. Patients’ individual needs were assessed with the help of screening instruments that measured the level of anxiety and depression and psychosocial risk factors: Hospital Anxiety and Depression Scale (HADS; German version: Herrmann-Lingen et al., 2011) and Psychosocial Risk Questionnaire (PRQ; Bussmann et al., 2023). Patients were allocated to a care level based on the screening instruments’ outcomes. Patients who show elevated symptoms of anxiety or depression were offered an appointment with psycho-oncologists (licensed psychotherapists). Highly distressed patients received a combination of PC and psychosocial care (with psychotherapists and psychosocial professionals). See Supplementary materials for more information on the stepped care model of the nfc-isPO and Kusch et al.’s (2022) publication on the overall concept.
The nfc-isPO was externally evaluated with a mixed-methods design (Jenniches et al., 2020; Krieger et al., 2020, 2021a, b, 2022). The aim was to gain comprehensive knowledge of all stakeholders’ experiences with the nfc-isPO to evaluate the quality of care and effectiveness (Jenniches et al., 2020). Postal patient surveys were conducted during its implementation at two points during patients’ yearlong care: 3 months and end of care (12 months). Each enrolled patient was contacted by the project Trust Centre, which was responsible for handling sensitive patient data according to German data protection laws, with a consent form and questionnaire by postal mail 3 months into enrolment. Dillman’s (1978) total design method was applied to achieve the highest possible response rate. Therefore, after 2 weeks, patients received a postcard with a reminder, while 3 weeks after the postcard, they received a reminder with a new questionnaire and consent form. The paper-based survey data were imported into SPSS (version 29) for later data analysis using the data-capturing software Teleform.
isPO service providers (e.g. psycho-oncologists) documented patients’ care in the documentation and assistance system CAPSYS2020, which was newly developed for the nfc-isPO. Patients who consented had pseudonymised care documentation regularly sent to a data warehouse and forwarded to the Trust Centre. Via a pseudonym list, selected variables from the CAPSYS2020 data set (e.g. sociodemographic characteristics) were linked to the survey data set.
The external evaluation design and data collection procedure were approved by the Ethics Committee of the University of Cologne (15.10.2018/18-092). Figure 2 overviews the described procedure.
Figure 2
Simplified overview of patient care paths and the data collection method (adapted version, Cecon-Stabel et al., 2023)
Note. Colour green represents pathways and data collection that is part of the care programme itself. Other colours (blue and grey) represent steps taken within the external evaluation design that are relevant for the presented research aim. Independent, dependent and mediator variable were collected in the patient survey. HADS – Hospital Anxiety and Depression Scale; PRQ – Psychosocial Risk Questionnaire.
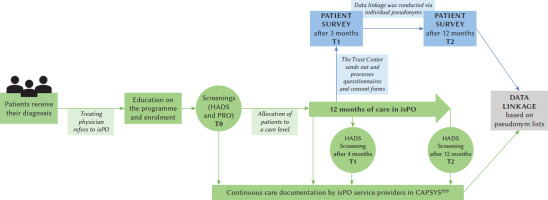
The patient surveys started in March 2019 and ended in July 2021. Due to the COVID-19 pandemic, recruitment issues occurred, and the project funder allowed patient care to be prolonged until March 2022 to achieve the sample size necessary for effectiveness analysis (Dresen et al., 2024). This extension did not apply to the patient surveys. Hence, not all patients who received care in isPO were contacted to participate in the T2 patient survey.
MEASUREMENTS
For sample characteristics, variables were linked from the CAPSYS2020 data set to the patient survey data set: age, sex, International Standard Classification of Education (isced) index and care network (pseudonymised via numbers 1 to 4). Further, the consultation dates were matched from CAPSYS2020 and the number of consultation was computed. Therapeutic alliance and SoC were included in the patient survey at T1 and T2.
Sense of coherence included the three subdimensions of comprehensibility (e.g. ‘Do you have a feeling that you are in an unfamiliar situation and don’t know what to do?’), manageability (e.g. ‘How often do you have feelings that you’re not sure you can keep under control?’) and meaningfulness (e.g. ‘How often do you have the feeling that there’s little meaning in the things you do in your daily life?’). They were measured using the validated 13-item version of the Sense of Coherence Scale (Cronbach’s α = .85; Schumacher et al., 2000). Participants indicated their (dis-) agreement on a 7-point semantic scale, with a total score ranging from 13 to 91. A higher score represented a stronger SoC (Antonovsky, 1987).
Therapeutic alliance was measured using the 12-item short German version of the Working Alliance Inventory (WAI-SR; Wilmers et al., 2008), based on the English WAI-SR (Hatcher & Gillaspy, 2006). Horvath and Greenberg (1989) developed and validated the original long version, which measured the dimensions of therapeutic alliance described by Bordin (1979). Bordin theorised that alliance comprised three aspects: agreement on therapy goals, agreement that therapy tasks address patients’ problems, and the interpersonal bond between patient and therapist. Hence, the scale included three subscales: goals (e.g. ‘My therapist and I collaborate on setting goals for my therapy’), tasks (e.g. ‘I feel that the things I do in therapy will help me to accomplish the changes that I want’) and bond (‘My therapist and I respect each other’). Participants indicated how often an item applied to them on a 5-point Likert scale (from seldom to always). Internal consistency is good, with Cronbach’s α between .81 and .91 for the subscales. For this study, two items of the WAI-SR were slightly adapted due to the context it was applied for. The items ‘What I am doing in therapy gives me new ways of looking at my problem’ and ‘I believe the way we are working with my problem is correct’ were changed to ‘What I am doing in therapy gives me new ways of looking at my way of dealing with the disease’ and ‘I believe the way we are working with how I deal with my cancer is correct’.
DATA ANALYSIS
Of all patients who enrolled in the nfc-isPO (N = 1,757), only patients treated by psycho-oncologists and who participated in both patient surveys and filled out the SoC scale were considered for analysis. Descriptive data analyses were performed with SPSS (version 29): stepwise, linear, multiple regression analyses were computed considering the subscales of therapeutic alliance (goals, tasks and bond) at T1 and the number of utilised consultations at T1 as independent variables to identify their influence and predict SoC at T2 (post-PC). An analysis was conducted for each subscale (comprehensibility, manageability and meaningfulness) and overall SoC. SoC at T1 was included as a control variable. The results were regarded statistically significant for p ≤ .05, with α = .05 as the significance level.
Results
SAMPLE DESCRIPTION
A total of 1,599 patients consented to be contacted and were invited to participate in the first survey (T1). As a result, 994 questionnaires were returned (response rate: 62.2%), of which 867 received a T2 questionnaire (see the explanation under Participants and procedure). As a result, 512 patients completed the T2 questionnaire (response rate: 59.3%). Of them, 220 received care from a psychotherapist and 102 filled out the SoC scale at T1 and T2. In the end, 100 filled out all three subscales (n = 101 for meaningfulness, n = 102 for comprehensibility and n = 101 for manageability).
The patients’ mean age was 54.97 years (SD = 10.85, min = 29.00, max = 83.00), and 78.4% (n = 80) identified as female (with 21.6%, n = 22, as male). According to the ISCED, 2% (n = 2) had a primary education level, 6.9% (n = 7) had a lower secondary education level, 60.8% (n = 62) had an upper secondary education level, 3.9% (n = 4) had a bachelor’s or an equivalent tertiary education level, 21.6% (n = 22) a master’s degree or an equivalent tertiary education level and 2.0% (n = 2) had a doctoral degree or equivalent tertiary education level (missing: n = 3). Moreover, 53.9% (n = 55) of patients were cared for in PC network no. 1. The other patients were distributed across the other three care networks (no. 2: n = 22; no. 3: n = 18; no. 4: n = 7). The three most common cancer diagnoses in our sample were breast cancer (35.3%, n = 36), lung/bronchial cancer (5.9%, n = 6) and rectal cancer (5.9%, n = 6).
Overall, SoC only increased slightly from T1 to T2 (see Table 1). However, the means differ across the subscales for T1 and T2 (Table 1). Meaningfulness has the highest mean values (T1: 5.03, T2: 5.12), manageability has the second highest (T1: 4.42, T2: 4.36) and comprehensibility has the lowest (T1: 3.89, T2: 4.14). Therapeutic alliance was rated between ‘most often’ and ‘very often’ at T1 (M = 3.85), indicating positive alliance, and ‘most often’ at T2 (M = 4.03; Table 1). The subscale bond was rated highest for T1 (M = 4.11) and T2 (M = 4.21), followed by goals (T1: 3.85, T2: 4.05) and tasks (T1: 3.40, T2: 3.84). The mean number of utilised consultations was 3.95 at T1 and 9.54 at T2 (Table 1).
Table 1
Mean values of SoC, therapeutic alliance and number of consultations at T1 and T2
MULTIPLE REGRESSION ANALYSES
All regression models show statistical significance: for overall SoC T2, F(5, 94) = 17.96, p < .001; for the subdimension of meaningfulness, F(5, 95) = 10.95, p < .001; for the subdimension of comprehensibility, F(5, 96) = 14.39, p < .001; for the subdimension of manageability, F(5, 95) = 14.96, p < .001. SoC at T1 and the subdimensions at T1 significantly predicted the level of SoC and the subdimensions at T2 in all regression models (Tables 2 and 3).
Table 2
Stepwise multiple regression analyses of sense of coherence at T1, therapeutic alliance and number of consultations at T1 as predictors and SoC at T2 as the dependent variable
Table 3
Stepwise multiple regression analyses of SoC at T1, therapeutic alliance and number of consultations at T1 as predictors and the SoC subdimensions of meaningfulness, comprehensibility, and manageability as dependent variables
The higher the therapeutic bond between the therapist and patient (therapeutic alliance–bond, T1) and the number of consultations (T1) were, the higher was the overall SoC at T2. 41.7% of the variation in the SoC at T2 is explained by the T1 value. Therapeutic bond and number of consultations add to the adjusted R2 by 4.4% (Table 2).
Apart from the SoC’s subdimension of meaningfulness at T1, only the number of consultations (T1) significantly predicts meaningfulness at T2. The higher the number of consultations was, the higher was the meaningfulness at T2, adding 4.7% to the explained variation of SoC T2 (Table 3).
For the SoC subdimension of comprehensibility, only its value at T1 predicts the T2 value in our models. Neither therapeutic alliance nor the number of consultations shows a significant influence (see Table 3).
For the SoC subdimension of manageability, therapeutic bond and goals at first significantly predict manageability at T2. Higher values in therapeutic bond (T1) result in higher values in manageability at T2. Therapeutic goals show a negative relationship, meaning lower values on the subscale (T1) seem to lead to higher manageability values at T2. However, the relationship between therapeutic goals and manageability becomes insignificant after the number of consultations is included in the model. Here, the number of consultations (T1) significantly predicts manageability at T2, meaning that the higher the number of consultations is, the higher is the manageability. Therapeutic bond (T1) and the number of consultations (T1) add 6.8% to the explained variance of manageability at T2 (Table 3).
Discussion
Based on newly diagnosed breast cancer patients’ survey data, Cecon et al. (2021) examined parts of the theory of salutogenesis in the context of psycho-oncology. They analysed the relationships of generalised resistance resources, SoC and tension; tension was defined as the subjective need for PC. Their results indicated that a strong SoC functions protectively and reduces the likelihood of developing the need for PC, hence utilising it (Cecon et al., 2021). According to the theory of salutogenesis, patients who develop tension – a need for PC – and utilise care services (tension management) are enabled to build up generalised resistance resources that positively affect their SoC and mental health.
As suggested by others (Hochwälder, 2022; Pfaff & Schmitt, 2023), examining a theory empirically is imperative to understand its quality and proposed causal effects. Our present analysis concurred. We focused on evaluating the components of tension management and SoC in the context of PC based on data from the nfc-isPO. Our results showed that in the nfc-isPO, therapeutic alliance partially predicted changes in cancer patients’ SoC during PC. When patients assessed therapeutic bond as better, SoC was higher at T2. However, subscale analyses revealed that this relationship only exists for manageability. Hence, therapeutic bond positively influenced the feeling that life stressors (e.g. cancer diagnosis and treatment) could be handled due to having sufficient coping resources.
Next, the number of consultations patients utilised – based on their individual needs – showed a significant relationship with SoC at T2. This relationship specifically applied to the subscales of meaningfulness and manageability. A higher number of consultations enhanced the feeling of being able to handle life stressors and promoted the perception that it was worthwhile to do so (meaningfulness).
Only a few studies have assessed the influence of psychotherapeutic interventions specifically on SoC. They have demonstrated that patients with mental health issues and persons belonging to vulnerable groups (e.g. unemployed individuals and older adults) showed an increase in SoC after receiving psychotherapeutic interventions (Humboldt & Leal, 2013; Langeland et al., 2006; Schäfer et al., 2020; Skärsäter et al., 2009; Szymona, 2005; Vastamäki et al., 2009). Langeland and colleagues (2007) conceptualised a promising group therapy intervention that integrated salutogenic principles to improve SoC, coping, and mental health. Those principles seem relevant for PC – which focuses on supporting patients with coping and minimising psychological and social problems in the context of their disease (Mehnert, 2014; Weis et al., 2007) – and probably overlap with what is already part of PC in practice. Moreover, a randomised controlled trial specifically showed a positive effect of a mindfulness-based stress reduction intervention on breast cancer patients’ SoC (Kenne Sarenmalm et al., 2017). However, overall, studies evaluating the path of effectiveness of psycho-oncological interventions on patients’ SoC are lacking. Reviews have shown a positive relationship between SoC and mental health and quality of life (Eriksson & Lindström, 2006, 2007). Researchers of salutogenesis have emphasised the necessity of conducting more research on how and to what degree SoC can be positively influenced (Hochwälder, 2022; Suominen & Lindstrom, 2008). Our results contribute to this research gap. Other study designs (e.g. dismantling designs) typically applied in psychotherapy research should be used to gain more detailed insight into this issue.
In all, our results align with research that shows positive effects of therapeutic interventions on SoC (Hojdahl et al., 2013; Humboldt & Leal, 2013; Kenne Sarenmalm et al., 2017; Schäfer et al., 2020; Skärsäter et al., 2009; Szymona, 2005; Vastamäki et al., 2009; Weissbecker et al., 2002). Qualitative evaluation data of the nfc-isPO support our quantitative results (Krieger et al., 2022): Patients who received care in the nfc-isPO and were interviewed on their care experiences identified a positive therapeutic alliance as facilitating for their PC, which resulted in overall care satisfaction (Krieger et al., 2022; Cecon-Stabel et al., 2024).
LIMITATIONS
SoC was included as a patient-reported outcome in the patient surveys, which focused on assessing indicators for quality of care (Cecon-Stabel et al., 2023). Only a fraction of patients who received psychotherapeutic care participated in both surveys, which led to a comparatively small sample size after matching T1 and T2 data. We cannot rule out that patients who participated in both surveys were likelier to be more motivated or have higher SoC or therapeutic alliance than non-participants.
Furthermore, the mean SoC did not change much from T1 to T2, and the SoC T1 value showed the highest explanatory power (adj. R2) for the T2 value. Other research suggests that persons with low SoC profit more from salutogenic interventions than persons with moderate to high SoC (Eriksson & Lindström, 2005; Hakanen et al., 2007). We cannot rule out sample selectivity or attrition bias due to individuals with lower SoC potentially being associated with non-participation in the survey or at T2.
Moreover, due to the survey design, we missed a T0 value: a value before PC started. As a result, possible changes between T0 and T1 were not considered in our analysis. We interpret these biases as conservative since they likely provided an underestimation of our results. Hence, individuals with lower SoC might have increased in SoC more from the intervention than those with average to high SoC.
Lastly, our results showed that the number of consultations positively predicted SoC. However, the cause of this significant relationship is unclear. For instance, specific topics covered in the consultations or therapeutic interventions the psychotherapists applied could have contributed to this result rather than the number of consultations. Therefore, a mixed-methods design, starting with qualitative methods followed by a quantitative evaluation, could help acquire insight into possible influential factors that act salutogenically.
Conclusions
In the context of PC, our results suggest that elements of successful tension management are a positive therapeutic bond and the number of needs-oriented consultations that are utilised. The SoC subdimensions of meaningfulness, comprehensibility and manageability are affected differently by these salutogenic factors. Our results contribute to research activities seeking to empirically evaluate components of the theory of salutogenesis. Nevertheless, more differentiated research is needed to discover paths of effectiveness to improve cancer patients’ mental health and SoC.
Supplementary materials are available on the journal’s website.


