BACKGROUND
Harmful use of alcohol is considered a major public health problem worldwide, considering that every year, 5.3% of all deaths result from harmful use of alcohol (World Health Organization, 2022). To characterize harmful use of alcohol, “alcohol use disorder” (AUD) was defined by the National Institute on Alcohol Abuse and Alcoholism as “a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational or health consequences” (National Institute on Alcohol Abuse and Alcoholism, 2023). AUD is also described in the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) as a disorder with multiple symptoms including spending a long time drinking, continuing to drink even if causing trouble with family or friends, and having to drink a lot more than before to get the desired effect (American Psychiatric Association, 2013).
Numerous children live with a parent who has an AUD, the rate being estimated around 10% of all children living in the USA (Lipari & Van Horn, 2017). Besides AUD, parental problem drinking includes symptoms of AUD and related difficulties such as parental hangovers, alcohol-related injuries and loss of job (Keller et al., 2022). In addition, several studies have shown the deleterious impact of parents’ alcohol dependence in offspring. Indeed, problematic parental alcohol use has been associated with adolescents’ substance use problems (Keller et al., 2022; Latendresse et al., 2008; Sternberg et al., 2018) and adolescents’ risky drinking with higher alcohol expectancies, i.e., to expect a positive effect of alcohol on mood (Homel & Warren, 2019; Zaso et al., 2023). Problematic parental alcohol use was also associated with adolescent conduct problems (Su et al., 2018). These consequences of problematic parental alcohol use for offspring were found to be even more significant when the degree of parent’s alcohol use was high (Sternberg et al., 2018; Wahlström et al., 2023). Moreover, in the context of problematic parental alcohol use, adolescents’ social relationships were reported to deteriorate, possibly due to a lack of self-confidence (Wahlström et al., 2023). Problematic parental alcohol use was also associated with higher perceived stress in offspring (Wahlström et al., 2023) and higher risk of psychopathology emerging during adolescence, notably generalized anxiety disorder (Oro et al., 2021).
While numerous studies have examined the effects of parental alcohol use on children (Keller et al., 2022, 2023; Su et al., 2018; Wahlström et al., 2023), much less attention has been paid to how parents themselves perceive and experience their own parenting in the context of alcohol use – an important yet underexplored aspect in the literature. This gap highlights the need to better understand the personal experiences of parents facing alcohol-related challenges.
To deepen the understanding of these subjective parenting experiences, it is essential to consider central constructs such as the parental sense of competence and parental burnout. The parental sense of competence refers to parents’ beliefs about their effectiveness and confidence in fulfilling their parenting role, which plays an important role, for example, for maintaining consistent parenting practices and supporting children’s emotional and behavioral development (Ohan et al., 2000; van Eldik et al., 2017). Parental burnout, characterized by emotional and physical exhaustion resulting from prolonged parenting stress, has been increasingly recognized as a significant factor influencing parenting behaviors (Mikolajczak et al., 2018; Sánchez-Rodríguez et al., 2019).
An important factor modulating the consequences of problematic parental alcohol use for offspring could be the parenting behavior (Latendresse et al., 2008). Parents’ AUD has been often linked to negative parental behavior such as “poor parenting”, including lack of caring attitudes, few activities shared between parent and child (e.g., playing together), and lack of fulfilment of parental responsibilities (Sternberg et al., 2018). Parental AUD has also been associated with “harsh parenting”, i.e., a continuum of attitudes with coercive acts and negative emotional expression (Bosk et al., 2021; Neppl et al., 2020). However, in the context of parental AUD, other studies have highlighted that positive parental behavior was associated with beneficial effects on offspring. For example, a report showed that, among mothers with AUD, the more maternal support was present for the child, the less AUD emerged in the child once they became an adult (Finan et al., 2018). This is in line with other studies showing that positive parental behaviors could modulate the negative effects of problematic parental alcohol use on offspring (Jääskeläinen et al., 2016; Latendresse et al., 2008). Another factor possibly regulating the consequences of problematic parental alcohol use could be the parental sense of competence of individuals with alcohol consumption. The parental sense of competence can be defined as parent’s perception of their ability to help their child to develop and grow positively (Ohan et al., 2000). A high level of parental sense of competence was found to be associated with positive parental behavior and family life satisfaction (van Eldik et al., 2017). A recent study exploring associations between alcohol use and parenting stress in mothers reported a significant but weak negative association between alcohol consumption and parenting sense of competence (Johnson et al., 2022). The authors thus suggested that, as a mother’s perception of her parenting sense of competence increases, her alcohol consumption tends to decrease (Johnson et al., 2022). Nevertheless, additional studies are required to substantiate this association.
Parenthood can be experienced as a difficult and challenging process, depending on several factors, including presence of psychopathological symptoms such as anxiety and/or depressive symptoms (Sánchez-Rodríguez et al., 2019) and insufficient social or family support (Amersfoort & Friesen, 2022; Mikolajczak et al., 2018). Indeed, studies showed that social and family support (e.g., having a “co-parent” who cooperates to manage children’s education) was associated with lower parenting stress, which could be due, for example, to the fact that a co-parent may provide the opportunity for the parent to rest and spend more “quality time” with their child (Durtschi et al., 2017; Mikolajczak et al., 2018). Regarding psychopathological symptoms, a qualitative study among mothers suffering from intense fatigue and anxiety reported high feelings of guilt about their parental attitudes and a low sense of parental competence (Hubert & Aujoulat, 2018). This study also suggested that maternal guilt could be associated with a lack of self-control and a tendency to react violently in some situations (Hubert & Aujoulat, 2018). In others studies, anxiety and depression symptoms were associated with parental “burnout”, including exhaustion, i.e., the parent feels immense emotional and physical fatigue (Mikolajczak et al., 2018; Sánchez-Rodríguez et al., 2019). Moreover, according to a longitudinal study, anxiety and depression symptoms, parental behavior and problematic parental alcohol use in adulthood may relate to stressors experienced in childhood and adolescence (Neppl et al., 2020). This suggested that associations could exist between post-traumatic stress disorder (PTSD) symptoms and parental AUD symptoms. PTSD symptoms are associated with experiencing a traumatic event, and defined by altered cognitions and mood, re-experiencing, avoidance strategies and high alert status, including increased arousal and reactivity (Ashbaugh et al., 2016). However, to our knowledge, no study has explored associations between PTSD symptoms and problematic parental alcohol use.
While several studies have highlighted the negative impact of problematic parental alcohol use on offspring’s mental health (Keller et al., 2022, 2023; Su et al., 2018; Wahlström et al., 2023), the perception of drinking parents about their parenting role remains poorly documented. This study thus aimed to assess the parental sense of competence among individuals with alcohol consumption and examine the relationship between psychopathological symptoms (anxiety, depression and PTSD), parental burnout, guilt, and social support. By focusing on subjective experiences of parents, the goal of this research was to provide an improved understanding of the factors influencing parenting behaviors, ultimately contributing insights for targeted interventions and better family outcomes. By focusing on the perceptions of parents with problematic alcohol consumption regarding their parenting deficits (e.g., parental sense of competence), this study could have important clinical implications. For instance, a recent study found that enhancing parents’ understanding of their parenting role and the support available to them during alcohol detoxification treatment significantly encouraged their engagement in therapeutic follow-up (Cioffi et al., 2023). This study is thus based, as a first step, on a comparative analysis between parents having low/no alcohol consumption with those having higher consumption. In a second step, to gain further insight into the typology of parents having problematic alcohol use, a cluster analysis was performed to identify profiles in the subsample of participants with higher alcohol consumption, the classification being based on levels of psychopathology symptoms. As demonstrated by previous studies, cluster analysis is particularly suited to this aim, as it enables the identification of distinct subgroups within a heterogeneous population, based on patterns of psychopathological symptomatology and alcohol consumption behaviors (Borsari et al., 2018; Dragan, 2020; Hawn et al., 2018; Lannoy et al., 2020). Moreover, by uncovering meaningful subgroups, cluster analysis can help to identify potential risk factors, tailor treatment approaches, and develop targeted intervention strategies for individuals within each cluster (Doron et al., 2015; Wemm et al., 2018). This study employed a cross-sectional design to explore associations between variables, acknowledging that this design does not allow for the determination of causal relationships.
CURRENT STUDY
The perception of drinking parents about their parenting role remains poorly documented. To address this gap, the current study aims to:
Assess the parental sense of competence among individuals with varying levels of alcohol consumption;
Examine the relationships between psychopathological symptoms (anxiety, depression, and PTSD), parental burnout, guilt, and social support in this population;
Compare parents with low or no alcohol consumption to those with higher consumption regarding these variables;
Perform a cluster analysis within the subgroup of parents with higher alcohol consumption to identify distinct profiles based on psychopathology symptoms.
PARTICIPANTS AND PROCEDURE
PARTICIPANTS
Participants were recruited via an advertisement posted on groups referenced on Facebook and focusing on various domains (fitness, outdoor, music, literature, cooking, home improvement, motherhood, etc.), as well as more general parents’ or support groups. The advertisements were also shared on personal Instagram accounts to encourage word-of-mouth promotion. The recruitment announcement was republished regularly, in order to obtain as many responses as possible. Potential participants were provided with a link to an online questionnaire on the LimeSurvey platform of University of Toulouse-Jean Jaurès. They were told that if they agreed to take part in the study, they would be asked to answer questions about their role as parents of young children and their alcohol consumption. To be eligible, participants had to be the mother or father of at least one child aged below 18 living at home. Each participant had to give their informed consent. The answers were anonymous, and participants did not receive compensation. The study protocol was approved by the local ethics committee and data protection officer of Research Ethics Committee of Toulouse University (file number 2022-481). APA ethical standards were followed regarding sample processing.
MEASURES
Personal information. Personal information was gathered including age, gender, educational level, occupational category, marital status, and parental and childcare status.
Parenting sense of competence. The parenting sense of competence was measured using a French language version of the Parenting Sense of Competence (PSOC) scale, a self-report inventory containing 17 items (Ohan et al., 2000; Trudelle & Montambault, 2005). An item example is: “Being a parent makes me tense and anxious”. As recommended (Gilmore & Cuskelly, 2009), items 1, 5, and 7 were suppressed to adapt the questionnaire to parents of children aged between 0 and 18 years old. Items were rated on a 4-point scale from 1 (strongly disagree) to 4 (strongly agree). Scoring for some items was reversed so that, for all items, higher scores indicated greater parenting sense of competence. PSOC is a widely used instrument and its psychometric properties were demonstrated by Ohan et al. (2000), showing acceptable to good reliability, with Cronbach’s α values ranging from .77 to .80. The Cronbach’s α value for PSOC was .81 in this study.
Parental burnout. Parental burnout was measured using the Parental Burnout Assessment (PBA), a self-report scale in which participants were provided with items regarding their role as parents (e.g., “I feel completely run down by my role as a parent”) and asked how often they have been bothered by the situation (Roskam et al., 2018). Answers were rated on a 7-point scale from 0 (never) to 6 (every day). Only the first 15 items (out of 22) of the PBA were answered by participants to preserve their resources for completing other scales of this study. Higher total scores suggested higher parental burnout. A previous study demonstrated excellent reliability of PBA, with a Cronbach’s α value of .96 (Roskam et al., 2018). The Cronbach’s α value for this scale was also .96 in this study.
Parental guilt. Parental guilt was measured using a three-item questionnaire (Sánchez-Rodríguez et al., 2019). An item example was: “I have regrets about some of my behaviors as a parent”. Responses were rated on a five-point scale from 1 (never) to 5 (every day). Higher total scores indicated higher parental guilt. A previous study demonstrated acceptable reliability of this questionnaire, with a Cronbach’s α value of .78 (Sánchez-Rodríguez et al., 2019). Cronbach’s α was .89 in this sample.
Alcohol consumption. Participant’s alcohol consumption was assessed with the three-item Alcohol Use Disorder Identification Test-C (AUDIT-C), a three-item self-report questionnaire (Bush et al., 1998; Gache et al., 2005). An item example was: “How often do you have 6 or more drinks on one occasion?” Responses were rated from 0 (never) to 4 (daily or almost daily). Higher scores indicated higher alcohol consumption. A total score of 4 or above was considered as a cutoff for possible heavy drinking and/or active alcohol abuse or dependence. The AUDIT-C is a widely used scale showing acceptable reliability in previous studies, with a Cronbach’s α value of .74 in a French sample (Choquette et al., 2018). Cronbach’s α was .77 in our study.
Perceived social support. Perceived social support was assessed using the Multidimensional Scale of Perceived Social Support (MSPSS), a 12-item self-report instrument (Denis et al., 2015; Zimet et al., 1990). An item example was: “There is a special person who is around when I am in need”. Items were rated on a 5-point scale from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicated higher perceived social support. The MSPSS is a frequently utilized scale showing good to excellent reliability in previous studies, with Cronbach’s alphas values ranging from .84 to .92 (Zimet et al., 1990). Cronbach’s α was .92 in this study.
Anxiety symptoms. Anxiety symptoms were measured using the Generalized Anxiety Disorder-7 (GAD-7), a self-report questionnaire in which participants are provided with a list of 7 symptoms (e.g., “Feeling nervous, anxious, or on edge”) and are asked how often they have been bothered by each symptom over the past 2 weeks (Micoulaud-Franchi et al., 2016; Spitzer et al., 2006). Answers were rated on a 4-point scale from 0 (never) to 3 (almost every day). Higher total scores indicated higher anxious symptomatology. The GAD-7 is a standard measurement scale showing good to excellent reliability in former studies, with Cronbach’s α values of .90 and .92, respectively (Micoulaud-Franchi et al., 2016; Spitzer et al., 2006). Cronbach’s α was .89 in this study.
Depression symptoms. Depression symptoms were assessed using a French language version of the Patient Health Questionnaire-9 (PHQ-9), a self-report questionnaire in which participants are provided with a list of 9 symptoms, e.g., “Feeling tired or having little energy” (Carballeira et al., 2007; Kroenke & Spitzer, 2002). Participants were asked how often they have been bothered by each symptom during the past 2 weeks. Answers were rated on a 4-point scale from 0 (not at all) to 3 (nearly every day). Higher total scores indicated higher depressive symptoms. The PHQ-9 is a broadly adopted scale showing good reliability in former studies, with Cronbach’s α values ranging from .86 to .89 (Kroenke et al., 2001). Cronbach’s α was .88 in this study.
Post-traumatic stress symptoms. Post-traumatic stress symptoms were measured using a French language version of the Post-traumatic stress disorder (PTSD) Checklist for DSM-5 (PCL-5), a self-report scale with 20 items (Ashbaugh et al., 2016). Respondents rated how much a problem described in the item (e.g., “Avoiding memories, thoughts or feelings related to experience”) had bothered them over the past month on a 5-point scale from 0 (not at all) to 4 (extremely). Higher total scores indicated higher PTSD symptoms. The PCL-5 is a widely used tool showing excellent reliability, with a Cronbach’s α value of .94 in a former study (Ashbaugh et al., 2016). Cronbach’s α was also .94 in this study.
DATA ANALYSIS
Data preparation. Eighteen participants were excluded from the study due to highly incomplete responses (over 5% missing data) or because they were not parents of a child under 18 living at home. For sporadic missing data, Little’s test was conducted to confirm that data were missing completely at random (Little, 1988). Missing data were imputed using the expectation-maximization algorithm. Data were screened for univariate outliers using z-scores, and for multivariate outliers through the Mahalanobis distance with p < .001 (Tabachnick & Fidell, 2007). Variables were checked for normality prior to analysis. A square root transformation was applied to total scores of parental burnout and AUDIT-C as both were positively skewed.
Statistical analyses. Comparisons between groups were made using the t-test. A cluster analysis was performed in two steps to identify distinct profiles of participants with higher alcohol consumption. The classification was based on the following variables: anxiety, depression, and PTSD symptoms. In the first step, a hierarchical cluster analysis was conducted to determine the optimum number of clusters in the sample, using Ward’s method with squared Euclidean distance, based on standardized total scores (z-score). The resulting dendrogram and agglomeration schedule were used to identify the number of clusters. As a second step, K-means clustering was used to assign each individual to the identified clusters. Statistical analyses were performed using IBM SPSS Statistics version 26.
Although the three clustering variables are likely correlated, principal component analysis was not applied prior to clustering. This decision was based on theoretical and methodological considerations: the three variables represent distinct and clinically meaningful dimensions of psychopathology, and combining them into principal components would reduce the interpretability of the clusters. Moreover, given the small number of variables (three), dimensionality reduction was not deemed necessary. Retaining the original variables allowed us to identify clusters that are directly interpretable in terms of mental health profiles relevant to parents with problematic alcohol use.
TRANSPARENCY AND OPENNESS
We report how we determined our sample size, all data exclusions, and all measures that were included in the analyses for this article. All data (including raw data) are available from the corresponding author by sending an email. Data were analyzed using IBM SPSS Statistics version 26. This study’s design and its analysis were not pre-registered.
RESULTS
SAMPLE CHARACTERISTICS AND DESCRIPTIVE STATISTICS
The sample was composed of 759 individuals including 708 women (93.3%), 38 men (5.0%) and 13 persons who did not indicate gender (1.7%). The mean age of the sample was 35.21 years (SD = 6.80). Other characteristics are shown in Table 1. Descriptive statistics of the whole sample are displayed in the left part of Table 2. Cronbach’s α values were in the acceptable to excellent range.
Table 1
Characteristics of the sample (mean age = 35.21, SD = 6.80, N = 759)
Table 2
Descriptive statistics of the whole sample and t-test comparison of the high alcohol consumption group (ALC) with the Control group (CTRL)
COMPARISON OF PARTICIPANTS WITH LOW OR HIGH ALCOHOL CONSUMPTION
An analysis was conducted to compare parents having low/no alcohol consumption with those having higher consumption, using an AUDIT-C total score above 3 as a cutoff. Participants scoring above 3 were thus assigned to the ALC group (n = 209, 90.3% women, 9.9% men), while those scoring below 4 were considered as the Control (CTRL) group (n = 550, 94.9% women, 3.3% men). The proportion of men was higher in the ALC group compared with the CTRL group (p = .001, Fisher’s exact test). Compared with the CTRL group, the ALC group was older, with a difference below 3 years of age (Table 2, right part). Regarding parenting variables, the ALC group had a lower score of perceived parental competence and higher scores of parental burnout and guilt, with statistical significance and small effect sizes (Cohen’s d). In terms of psychopathology, the ALC group had higher scores of anxiety, depression, and PTSD symptoms in comparison to the CTRL group, with statistical significance and small to medium effect sizes. Regarding perceived social support, the difference between groups was not significant. These results thus suggested that individuals with higher alcohol consumption had more degraded feelings of their role as parents and worse mental health when compared with those with lower drinking.
CLUSTER ANALYSIS OF THE ALC GROUP
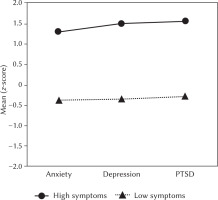
To gain further insight in the typology of parents with higher alcohol consumption, a cluster analysis was performed in the ALC group. The classification was based on scores in psychopathology symptoms, i.e., anxiety, depression, and PTSD. In the first step, a hierarchical cluster classification was performed to identify the optimal number of clusters of this subsample, based on the dendrogram and the agglomeration schedule. The dendrogram clearly indicated a two-cluster solution (Figure 1). Supporting this solution, the agglomeration schedule showed a sudden increase in linkage distance, with a difference value of 367.3, when two clusters merged to a single cluster, while the passage from three to two clusters had a difference of only 54.9. This indicated that the passage from two clusters to a single one would have a much greater impact on cluster heterogeneity than previous stages of the analysis, indicating that a two-cluster solution was the most appropriate to classify the ALC group. In the second step, K-means clustering was used to assign each individual to one of the two clusters. Once this step was completed, a discriminant function analysis was conducted to evaluate the internal validity of the cluster solution. The analysis revealed significant differences between the clusters (Wilks’ λ = 0.28, p < .001), and a high reclassification accuracy, with 98.6% of cases correctly assigned to their respective cluster. This strongly supported the reliability and stability of the identified two-cluster structure within the ALC group. In addition, to address potential bias introduced by imputed values, a sensitivity analysis was conducted by repeating the cluster analysis on a reduced dataset including only complete cases. The results confirmed the stability of the two-cluster solution, with nearly identical z-scores across datasets (Table S1 and Table S2 in Supplementary materials).
Figure 1
Hierarchical clustering dendrogram of the ALC group using Ward linkage with squared Euclidean distance
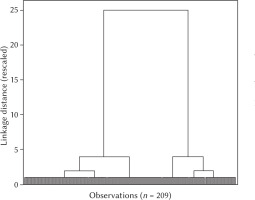
To represent the profile of these two clusters regarding their levels of anxiety, depression, and PTSD symptoms, the mean (z-score) of each symptom score was plotted (Figure 2). The top cluster was called “High symptoms” (H, n = 69, 33.0%) as it was composed of participants whose scores of anxiety, depression, and PTSD symptoms were almost one and a half standard deviations (SDs) above the mean. The bottom cluster was called “Low symptoms” (L, n = 140, 66.9%) as it comprised individuals whose scores of anxiety, depression, and PTSD were less than half an SD below the mean.
Next, these clusters were compared to each other using the t-test (Table 3). Regarding anxiety, depression, and PTSD symptoms, significant inter-cluster differences were found, with very large effect sizes, which further validated the classification. Regarding parenting variables, the H cluster had a lower score of sense of competence and higher scores of burnout and guilt in comparison with L, with statistical significance and large effect sizes. The H cluster also showed lower perceived social support and higher alcohol use, and was somewhat younger than the L group. Taken together, these results suggested that, within the subsample of parents with higher alcohol consumption, two highly distinct groups can be identified based on their level of psychopathology symptoms and feelings of their role as parents: a group with high symptoms and poor parenting experience; and a group with low symptoms and more positive parenting experience.
Table 3
Cluster analysis of the ALC subsample with higher alcohol consumption (n = 209); cluster comparison using t-test
DISCUSSION
This study examined associations between feelings of parental role (including parental sense of competence, parental burnout symptoms, and parental guilt) and psychopathological symptoms (i.e., anxiety, depressive and PTSD symptoms) in parents who drink alcohol. This study is based, firstly, on a comparative analysis between parents having low/no alcohol consumption and those having higher consumption. Secondly, to gain further insight into the typology of parents with significant alcohol consumption, a cluster analysis was performed. The internal consistency of measures, as indicated by Cronbach’s α values, ranged from acceptable to excellent, reinforcing the reliability of the data collected. Exclusion criteria for incomplete participant responses, identification of missing data patterns, imputation techniques, outlier screenings and normalization protocols fortified the integrity of the subsequent analyses.
COMPARATIVE ANALYSIS
In the comparative analysis, parents with higher alcohol consumption (ALC group) exhibited notable differences compared to those with low/no alcohol consumption (CTRL group). The decision to categorize parents into low/no alcohol consumption and higher alcohol consumption groups was driven by the interest in highlighting key sociodemographic, parental, and psychopathological differences. Firstly, in terms of sociodemographic variables, one notable distinction was the higher proportion of men in the ALC group compared to the Control group, with statistical significance. This is consistent with worldwide alcohol consumption being higher for men than women (World Health Organization, 2022) and with a study reporting that women living with children consumed significantly less alcohol than men living with children (Graham et al., 2020). This is also convergent with a report showing that parental responsibilities could be a protective factor against alcohol consumption in mothers, but not in fathers (Kuntsche et al., 2012).
In terms of parenting variables, the diminished sense of parental competence in members of the ALC group suggested a negative perspective on their role as parents. This is in agreement with a study reporting a significant, weak negative association between alcohol consumption and parenting sense of competence (Johnson et al., 2022). Our results also align with a recent study in individuals affected by AUD, where self-perception tended to be adverse, often associated with a profound sense of shame associated with alcohol consumption (Milan & Varescon, 2022). Our findings thus echo this pattern, showing that significant alcohol consumption was associated with a decreased sense of parental competence, potentially impacting their perception of their ability to support their child’s development. It should be noted that lower parental competence ratings in the higher alcohol consumption group might be partly influenced by underlying psychopathology, such as depressive symptoms, which are known to negatively bias self-evaluations (Mehrizi et al., 2023). Future research could use mediation analyses to clarify the role of alcohol consumption in the relationship between psychopathology and perceived parental competence.
Additionally, the ALC group exhibited heightened parental burnout symptoms compared to the Control group, suggesting greater emotional and physical fatigue. Previous studies have linked AUD symptoms with difficulties in emotional regulation (Cavicchioli et al., 2020; Stellern et al., 2023), which may help explain the association between higher alcohol consumption and parental burnout. Moreover, alcohol may serve as a coping mechanism for parental burnout symptoms, as suggested by research on drinking to manage stress (Corbin et al., 2013). However, its specific role in parental burnout remains underexplored (Cook et al., 2022; Roskam & Mikolajczak, 2021).
In addition, the observed association between parental alcohol use and elevated burnout symptoms raises the question of social outlook among parents concerned by higher alcohol consumption. Indeed, research indicated that the societal expectation to conform to the standards of being a “good parent” was associated with elevated burnout symptoms, encompassing emotional exhaustion and negative parenting experiences (Roskam & Mikolajczak, 2021). Consequently, parents who consume alcohol might feel that their behavior places them outside social norms, intensifying feelings of burnout.
This could also align with higher mean scores of parental guilt noted in the ALC group, which could be associated with impaired self-control reported in individuals with problematic alcohol use (Stellern et al., 2023). This guilt might arise from concerns about impulsive behaviors detrimental to offspring, although evidence on the link between guilt and AUD is mixed (Milan et al., 2023). Nonetheless, elevated guilt in this context may also reflect parents’ engagement and concern for their parenting role, despite potential impairment from drinking.
Moving on to psychopathological factors, the ALC group exhibited higher scores of anxiety, depression, and PTSD symptoms compared to the Control group, suggesting that parents with higher alcohol consumption not only perceive themselves as less competent parents but also experience more significant mental health challenges. In addition, higher psychopathology symptoms in ALC appeared to be convergent with former studies showing that, in the general population, heavy drinkers had higher depression levels, even though these reports also identified U/J-shaped relationships where abstainers had higher depression scores than light drinker (Gémes et al., 2019; Rodgers et al., 2000). Our results also appear to be consistent with studies in young adults reporting associations between higher AUD symptoms and traumatic events (Cusack et al., 2023) and showing that depression and PTSD symptoms were associated with higher demand for alcohol in an alcohol purchase task (Murphy et al., 2013).
These findings can be further understood in light of the transactional model of stress and coping, originally developed by Lazarus and Folkman (1984) and recently updated by Folkman (2020). This model posits that individuals respond to perceived stress through coping mechanisms shaped by personal and contextual factors. In this framework, parents experiencing emotional exhaustion or negative self-perceptions may turn to alcohol use as a maladaptive strategy to regulate stress or emotional distress, particularly when other coping resources are lacking. Recent research by Senn et al. (2023) supports this framework, showing that parental stress mediates the effects of parental risk factors (e.g., depressive symptoms) on dysfunctional parenting in first-time parents, highlighting the complex interplay between stress, coping, and parenting outcomes.
Cluster analysis of the ALC group
THE SECOND PART OF THE STUDY EXPLORED THE TYPOLOGY OF PARENTS WITHIN THE SUBSAMPLE EXHIBITING HIGHER ALCOHOL CONSUMPTION (ALC GROUP), USING CLUSTER ANALYSIS TO IDENTIFY DISTINCT PROFILES BASED ON PSYCHOPATHOLOGY SYMPTOMS SUCH AS ANXIETY, DEPRESSION, AND PTSD. THIS PERSON-CENTERED APPROACH ALLOWED US TO MOVE BEYOND MEAN-GROUP COMPARISONS AND IDENTIFY DISTINCT PSYCHOLOGICAL PROFILES THAT MAY UNDERLIE DIFFERENT TRAJECTORIES IN PARENTING AND ALCOHOL USE.
The analysis used a two-step process, starting with hierarchical cluster classification and followed by K-means clustering, to determine the optimal number of clusters. The dendrogram from the hierarchical cluster analysis revealed a clear two-cluster solution (Figure 1), substantiated by a significant increase in linkage distance when merging clusters. This suggested that a two-cluster solution was the most suitable for classifying the ALC group. K-means clustering was then employed to assign individuals to these two clusters, and subsequent discriminant analysis showed significant differences between the clusters, with a high accuracy of 98.6% in classification.
To elucidate the characteristics of these clusters concerning anxiety, depression, and PTSD symptoms, the study plotted the mean (z-score) of each symptom (Figure 2). The top cluster, labeled “High symptoms” (H), comprised participants with scores well above the mean, while the bottom cluster, labeled “Low symptoms” (L), included individuals with scores below the mean. Further analysis, including t-tests, highlighted significant inter-cluster differences in psychopathology symptoms, confirming the validity of the classification.
Moving beyond psychopathology, the cluster analysis extended its scope to parenting-related variables. Thus, the H cluster exhibited lower scores in sense of parental competence, higher levels of parental burnout and guilt, lower perceived social support, higher alcohol use, and a slightly younger demographic compared to the L cluster. These differences were not only statistically significant but also accompanied by large effect sizes, reinforcing the robustness of the findings. These associations underline the clinical relevance of the cluster solution, as the profiles combine psychological distress with parenting difficulties, painting a more comprehensive picture of vulnerability within the ALC group.
The typology emerging from the clusters highlights differentiated profiles of parental experience, notably one cluster characterized by high levels of psychopathological symptoms and a negative parenting experience, such as elevated parental burnout. This typological differentiation aligns with certain theoretical models, such as Gross’s emotion regulation framework (Gross, 2015) and Roskam and Mikolajczak’s (2021) parental burnout model. Parents in this high-symptom cluster may be more likely to adopt maladaptive emotion regulation strategies, including alcohol use, in response to parenting-related stress and limited social support. This typology provides valuable insights into how certain psychological and contextual vulnerabilities may co-occur in specific patterns among parents with elevated alcohol consumption.
In essence, the cluster analysis suggested that, within the subset of parents with higher alcohol consumption, there are two distinct groups: one characterized by higher psychopathology symptoms and negative parenting experiences, and the other characterized by lower psychopathology symptoms and more positive parenting experiences. To our knowledge, this is one of the first studies to apply a cluster-analytic approach to parents with elevated alcohol use, integrating both psychopathological and parenting dimensions. This typological perspective offers a novel contribution to the literature. By uncovering subgroups with distinct constellations of psychological and parenting characteristics, our findings may inform the development of more personalized intervention strategies aimed at supporting both parental mental health and parenting functioning.
LIMITATIONS
This study is not without limitations. Firstly, the reliance on self-report measures, especially for sensitive topics like alcohol consumption and mental health, may introduce response bias. Participants may underreport or overreport certain behaviors due to social desirability or recall bias. Another limitation could stem from selection bias in participant recruitment, potentially discouraging individuals with serious concerns about their alcohol use or those who feel highly incompetent in their parenting roles from participating in the study. Thirdly, the notable imbalance in the gender ratio, with a significantly higher proportion of women participants, introduces a limitation regarding the generalizability of the study’s findings, even though an uneven gender ratio is convergent with others studies about parenthood (Graham et al., 2020; Hagerman et al., 2020; Mikolajczak et al., 2018). This raises concerns about the extent to which the study’s conclusions can be applied to both genders equally, and thus future research with a more balanced representation of both genders is necessary. Fourthly, the cross-sectional design of the study limits the ability to establish causal relationships. As a result, it is not possible to identify a direct causal link between alcohol consumption, parental variables, and mental health variables. For instance, it remains unclear whether alcohol consumption leads to low feelings of parental competence or is a consequence of them. Nevertheless, the study also presents methodological strengths, particularly the combined use of comparative and cluster approaches. This dual strategy enabled a clearer characterization of the heterogeneity within the population and of the relationships between alcohol use, parenting and mental health.
EMERGING PERSPECTIVES AND CLINICAL IMPLICATIONS
Future research could employ longitudinal designs to explore causal relationships between alcohol consumption, parental role variables, and psychopathological symptoms. This would clarify whether alcohol use exacerbates parenting challenges or if parenting stressors drive increased consumption. In addition, investigating mediating factors, such as emotional regulation, social support, or stigma related to parenting and alcohol use, could help identify pathways that connect alcohol consumption to burnout, guilt, and competence perceptions. Furthermore, future studies could investigate the role of societal expectations and stigma in exacerbating guilt and burnout among parents with alcohol use concerns.
In terms of clinical implications, the distinct profiles revealed by the cluster analysis highlight the need for targeted interventions. Programs could be tailored to the unique needs of parents in the high-psychopathology cluster, focusing on emotional regulation, mental health treatment, and parenting skills, while also addressing alcohol-related behaviors. In addition, interventions aimed at reducing stigma may help alleviate emotional strain and improve parenting outcomes. For example, these interventions could take the form of support groups specifically for parents struggling with alcohol-related guilt or integrated therapeutic programs combining parenting support with addiction counseling. Collaborations between mental health professionals and addiction specialists could also help ensure early identification and holistic support.
CONCLUSIONS
Despite its limitations, the study provides valuable insights into connections between parenting, alcohol consumption, and mental health. The comparative analysis revealed significant distinctions between parents with low/no alcohol consumption and those with higher consumption, as the latter exhibited lower perceived parental competence and higher levels of parental burnout and guilt, signifying a more challenging perception of their role as parents. The elevated level of psychopathological symptoms in the group of parents with higher alcohol drinking indicated that members of this group not only perceived themselves as less competent parents but also they experienced more mental health challenges. However, the subsequent cluster analysis within this group identified two distinct clusters, one characterized by higher psychopathology symptoms and negative parenting experiences, and the other characterized by lower psychopathology symptoms and more positive parenting experiences. This nuanced typology emphasizes the need for a more personalized understanding of the intersection between parenting, alcohol consumption and mental health. These findings hold implications for interventions and support strategies tailored to specific needs of parents concerned with alcohol consumption and associated psychosocial challenges.
Supplementary materials are available on the journal’s website.