BACKGROUND
Early prevention is an important feature of medicine and a promising strategy for reducing mental and physical health problems. Developed countries are more likely than developing countries to have national policies for early prevention resulting in better health outcomes and improved quality of life. Innovative efforts to promote early prevention in developing countries, such as Armenia, is a cornerstone of global health. Historically, in behavioral and mental health research, early intervention programs were designed to detect and intervene to prevent the onset of delinquent behavior (Conroy & Brown, 2004; Loeber, 2003). Since then, applications of these programs have been generalized to address a wide range of conditions, including those associated with risk for sexual dysfunctions.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5; APA, 2013) defines sexual dysfunctions as “a heterogeneous group of disorders that are typically characterized by a clinically significant disturbance in a person’s ability to respond sexually or to experience sexual pleasure.” The DSM-5 has specific listings for seven sexual dysfunctions: delayed ejaculation, erectile disorder, male hypoactive sexual desire disorder, premature (early) ejaculation, female orgasmic disorder, female sexual interest/arousal disorder, genito-pelvic pain/penetration disorder, and substance/medication-induced sexual dysfunction. The International Classification of Diseases (ICD-11; WHO, 2022) classifies sexual dysfunctions under conditions related to sexual health, and conceptualizes these conditions as follows: “Sexual dysfunctions are syndromes that comprise the various ways in which adult people may have difficulty experiencing personally satisfying, non-coercive sexual activities. Sexual response is a complex interaction of psychological, interpersonal, social, cultural and physiological processes and one or more of these factors may affect any stage of the sexual response.” The ICD-11 listings for sexual dysfunctions include: hypoactive sexual desire dysfunction, sexual arousal dysfunctions, orgasmic dysfunctions, and ejaculatory dysfunctions.
The Adverse Childhood Experiences (ACE) Study, conducted at Kaiser Permanente in collaboration with the Centers for Disease Control and Prevention, is one of the first large scale studies demonstrating how early adversities can have long lasting effects on mental and physical health (Felitti et al., 1998). The original study involved over 17,000 patients who completed a survey as a part of their routine examination consisting of 10 questions about traumatic experiences that had occurred before the age of 18 as well as their current health status and behaviors. The ACE items consisted of three items related to abuse (physical, emotional, sexual), two items related to neglect (physical and emotional), and five items related to household dysfunctions (caregiver’s mental illness, incarcerated relatives, substance abuse, mother treated violently, parents separated or divorced). The main findings of the study were as follows: 1) ACEs were common, with two-thirds of the patients reporting at least one ACE, and more than one in five reporting three or more ACEs, 2) there was a graded or dose-dependent association between ACEs and negative health; as ACE scores increased, so did the risk for mental and physical problems. Since the original ACE study, researchers across disciplines have examined the relationship between ACE and health outcomes ranging from childhood problems all the way to mortality (Brown et al., 2009; Kelly-Irving et al., 2013). More recently, efforts have focused on cultural and societal aspects of childhood adversity, leading to the development of the Adverse Childhood Experiences International Questionnaire (ACE-IQ; WHO, 2018).
The relationship between adverse childhood experiences and poor health outcomes has been studied in many countries, including former Soviet republics as well as regional and neighboring countries of Armenia, such as Russia, Turkey, Moldova, Iran, and Ukraine. World Health Organization (WHO) reports from Russia, Turkey, and Moldova found that ACEs were common in these countries. In Russia, 84.6% of responders reported at least one, 28.2% reported at least two, and 17.5% reported four or more ACEs (Kachaeva et al., 2004). Furthermore, four or more ACEs were associated with an increase in the odds of smoking (OR = 2.10), harmful alcohol use (OR = 10.40), drug abuse (OR = 11.90), risky sexual behaviors (OR = 1.70), unwanted pregnancy (OR = 7.90), and attempted suicide (OR = 23.20). The results from Turkey were similar with respect to the commonality of ACEs, with 49.7% reporting experiencing at least one ACE, 26.1% reporting at least two, and 7.1% reporting four or more ACEs (Ulukol et al., 2014). ACE scores were positively associated with adverse health outcomes; four or more ACEs were associated with increased odds of smoking (OR = 3.69), alcohol (OR = 4.46) and drug (OR = 9.69) use. Finally, the WHO report from Moldova revealed the following: 59.6% reported experiencing at least one ACE and 12.5% reported four or more ACEs (Leco et al., 2018). Consistently with the other reports, ACE scores were positively associated with adverse health outcomes; four or more ACEs were associated with an increase in smoking (OR = 1.78), alcohol consumption (OR = 1.40), driving under the influence (OR = 2.83), injecting drug use (OR = 20.06), drug use (OR = 2.41), and suicide attempts (OR = 9.55). A study from Iran showed a significant correlation between ACEs and suicide (r = .32), substance abuse (r = .18), alcohol consumption (r = .22), cigarette smoking (r = .24), and other stress drugs (r = .17) (Kiani et al., 2019). Another study from Ukraine also found that ACEs were common: 44.7% reported 1-2 ACEs, and 9.5% reported three or more ACEs. Subjects with three or more ACEs were most likely to have chronic pain (OR = 3.60), cardiovascular disease (OR = 2.17), other disease (OR = 2.05), depressive disorders (OR = 1.93), anxiety disorders (OR = 3.04), and substance abuse disorders (OR = 2.35) (Fowler et al., 2020). Taken together, international research shows that ACEs are common and have implications for health and wellbeing.
Although the link between ACEs and poor health outcomes has long been established across the world, less is known concerning the relationship between childhood adversities and specific sexual dysfunctions. The etiology of sexual dysfunction is conceptualized as having multiple causes, including biological and environmental factors. The relationship between environmental risk factors and sexual dysfunctions has been implicated in male premature ejaculation and low sexual desire (Kinzl et al., 1995), sexual dissatisfaction and difficulties (Bigras et al., 2017), and sexual offending and paraphilic disorders (Levenson & Socia, 2016). One specific type of sexual dysfunction where less is known is the relationship between genito-pelvic pain/penetration disorder, formerly known as dyspareunia and vaginismus. Although the effects of child sexual abuse alone on this condition have been explored in other studies (Lutfey et al., 2008; Staples et al., 2012), given that ACEs include child sexual abuse as well as other adversities, the use of ACE may have important clinical implications for preventing and treating this condition. Further, no studies have examined the prevalence of ACEs and their associations with health outcomes in Armenia. Armenia’s history and culture, ethnic composition, conservative family model, and the geopolitical situation, especially in light of the second Artsakh (Nagorno-Karabakh) war, make it a region in great need of research.
This promoted the formulation of two research questions aimed at understanding the role of ACEs in sexual dysfunctions: 1) how common are ACEs in female patients with sexual dysfunctions, and 2) what are the most common types of ACEs in female patients with sexual dysfunctions? We hypothesized that patients with sexual dysfunctions would have more ACEs in comparison to control subjects. We also hypothesized that traumatic experiences relating to emotional, sexual, and physical abuse would occur with a greater frequency than neglect and household dysfunctions.
PARTICIPANTS AND PROCEDURE
PARTICIPANTS
Participants for the control group (n = 221) were recruited through a nonrandom convenience sample of medical students, healthcare workers, acquaintances and friends of the investigators, and other community volunteers mainly from Yerevan, capital of Armenia. Participants for the sexual dysfunction group consisted of patients (n = 85) from the Clinic of Sexology at Yerevan State Medical University. The response rate for both groups of subjects who voluntarily agreed to participate was over 90%. The demographic characteristics are shown in Table 1. Demographic variables included age (grouped in four cohorts: < 25, 26-35, 36-45, > 46), sex (male, female), marital status (single, married, divorced, widow), education (high school, vocational, higher education), and residential setting (city, village, town).
Table 1
Sample demographics
MEASURES
Adverse Childhood Experience (ACE) Questionnaire. An Armenian translated version of the ACE questionnaire based on the Felitti et al. (1998) study was used to measure childhood adversities. Three categories of childhood adversities consisting of nine items were measured: three items related to abuse (physical, emotional, sexual), two items related to neglect (physical and emotional), and four items related to household dysfunctions (caregiver’s mental illness, incarcerated relatives, substance abuse, mother treated violently). All questions were binary (no – 0 or yes – 1) and pertained to the respondents’ first 18 years of life. The total ACE score was calculated by summing the 10 questions for a possible total score between 0 (no exposure) and 10 (higher scores indicating more exposure).
The Changes in Sexual Functioning Questionnaire (CSFQ). The patient group was assessed with the ACE questionnaire as well as an Armenian translated version of the CSFQ based on Clayton et al. (1997) to measure illness and changes in sexual functioning. CSFQ is a 36-item semi-structured interview/questionnaire consisting of five subscales: sexual pleasure, frequency, interest, arousal, and orgasm. Key items are rated on a 5-point Likert scale where the patient is asked to rate changes in sexual functioning.
DATA COLLECTION
The data were collected by the first author and medical residents from community volunteers and the Clinic of Sexopathology. Control participants were asked to complete the ACE questionnaire in a self-administered format, whereas patients were assessed in an interview format. The study was approved by the Research Ethics Committee of the Yerevan State Medical University (no. YSMU2019RA_325).
DATA ANALYSIS
Descriptive statistics were computed for the demographic variables as well as the questionnaire items for each group. The chi-square test was used to assess group differences in demographic characteristics. Given that the number of male participants was low in the patient group, statistical analyses were carried out using female participants from both groups only. As the ACE score was not normally distributed, non-parametric tests were used to test the hypothesis. The Mann-Whitney non-parametric test was used for group comparisons of ACE items. The odds ratio (OR) was used to estimate the risk between ACE and sexual dysfunctions. Spearman correlation was used to evaluate the connection between ACE score and adverse health outcomes. The Kruskal-Wallis non-parametric test was used to explore the influence of ACE scores on sexual dysfunctions. Statistical analyses were conducted using SPSS 22 for Windows.
RESULTS
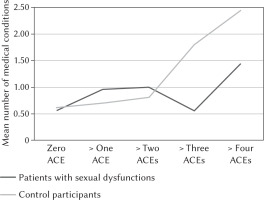
Table 1 presents age, sex, education levels, marital status, and residential settings for the total sample. There was no statistically significant difference between female patients with sexual dysfunctions and female controls in age (U = 5511.53, p = .116), though there was a significant difference in education levels (χ2(2) = 14.41, p < .001), marital status (χ2(2) = 66.45, p < .001), and residential settings (χ2(2) = 21.24, p < .001). Table 2 presents the proportion of patients and controls reporting “yes” to each ACE questionnaire items. In comparison to controls, patients reported a higher rate of growing up in a household with divorced or absent parents (42%) (χ2(1) = 7.58, p = .009, V = 0.18] and witnessing the mother being abused (27%) (χ2(1) = 76.64, p = .142, V = 0.17). The means, standard deviations, medians, and range for the ACE total score are presented in Table 3. The total ACE score was higher in patients (M = 2.06, SD = 1.95) than controls (M = 1.65, SD = 2.05) (U = 5246.01, p = .033, η2 = 0.02). Figure 1 shows the proportion of participants who reported exposure to none, or at least one, two, three or more than four ACEs. Three quarters (75%) of the patients reported exposure to at least one ACE and almost two-thirds (27%) reported exposure to four or more ACEs. In comparison, control participants reported lower rates of exposure to childhood adversities in general, with only 15% experiencing four or more ACEs. Figure 2 presents the percent of the participants who reported having at least one medical and/or co-occurring psychiatric condition. There was no group difference between the two groups in the number of these conditions. The most commonly self-reported co-occurring medical and/or psychiatric conditions in the patient group were headache (57%), sleep disturbance (48%), depression (17%), respiratory problem (12%), thyroid disease (12%), and kidney disease (10%). Thirty percent of the patients had more than one co-occurring condition. In the control group, co-occurring medical and/or psychiatric conditions included headache (51%), sleep disturbance (33%), depression (26%), thyroid disease (12%), and skin disease (11%). There were also some rare conditions (< 5%) in both groups such as anemia, infectious disease, and blood disease. There was a significant difference between the ACE score and the presence of medical conditions in the control group (U = 1797.47, p < .001, η2 = 0.12), but no significant difference was found for the patients. A correlation between ACE scores and the number of additional conditions was found in the control group (rs = .40). Female control participants exposed to ACEs were more likely to have kidney failure (U = 32.01, p = .002, η2 = 0.09) or sleep disorder (U = 372.54, p = .008, η2 = 0.09). Furthermore, ACE was significantly higher among controls who had depression (p < .01), headaches (p < .01), and thyroid dysfunctions (p < .05), compared to those who did not.
Table 2
Percentage of female participants responding “yes” to ACE item
Table 3
Mann-Whitney U test for ACE total score between female patients with sexual dysfunctions and control participants
| M | 95% CI | SD | Me | IQR | Range | Mann-Whitney U test | p | η2 | |
|---|---|---|---|---|---|---|---|---|---|
| Patients with sexual dysfunctions | 2.06 | 1.63-2.49 | 1.95 | 1.00 | 4 | 0-6 | 5246.01 | .033 | 0.02 |
| Control participants | 1.65 | 1.32-1.97 | 2.05 | 1.00 | 3 | 0-8 |
Figure 1
Percentage of participants with zero, or at least one, two, three, four or more ACEs
Note. ACEs – adverse childhood experiences.
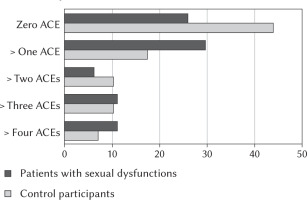
Figure 2
ACEs graded dose-dependent (x axis) relationship with increase in the number of medical conditions (y axis) for patients with sexual dysfunctions and control participants
Note. ACEs – adverse childhood experiences.
The most common sexual disorder diagnoses were: genito-pelvic pain/penetration disorder (81.5%), dyspareunia (8.6%), anorgasmia (6.2%), and absence of sexual desire (3.7%). ACE scores did not differ significantly based on diagnosis (χ2(3) = 2.69, p = .441). Table 4 presents the median and the percent of responses for CSFQ items that reflect problems in sexual functioning. One-third of the patients reported little to no enjoyment in orgasm, sexual thoughts, and sexual life. Similarly, one-third reported never or rarely experiencing sexual arousal. Patients with three or more ACEs were more likely to report problems in sexual arousal. There were no other differences or associations between number of ACEs and changes in sexual functions.
Table 4
Patient responses to items from Changes in Sexual Functioning (CSFQ) questionnaire
[i] Note. The CSFQ-14 uses a 5-point Likert scale to measure changes in sexual functioning. The answers for some of the items range from never to every day or no enjoyment to great enjoyment. We assigned each response a point value, from 1 to 4, with lower values reflecting problematic sexual functioning. The exception is question number 33 – the experience of painful intercourse – where a higher value reflects a greater problem
DISCUSSION
Our study found that female patients with sexual dysfunctions were exposed to more childhood adversities compared to control participants. Female patients with sexual dysfunctions reported higher total ACE scores (2.06 compared with 1.65 for controls), suggesting that environmental factors constitute a pathogenic basis for sexual dysfunctions. Among both groups, there were small but positive associations between childhood adversities and poorer health outcomes. However, this finding was significant only for control participants. The overall prevalence of ACE in our sample was similar to rates reported in other international studies. ACEs were common among all participants; 74.1% of the patient group reported at least one, 44.4% reported at least two, and 27.2% reported four or more ACEs. The numbers were lower in control participants; 56.1% reported at least one, 38.7% reported at least two, and 18.1% reported four or more ACEs.
In comparison to controls, patients with sexual dysfunctions were twice as likely to report parental divorce (OR = 2.20) and witnessing the mother being abused (OR = 2.40). We hypothesize that parental divorce and witnessing the mother being abused may lead to anxious feelings and affect a child’s perception about relationship stability. Consequently, later in life, this can interfere with intimacy and the ability to experience sexual pleasure. This hypothesis is consistent with comorbidity research indicating that mood and anxiety disorders are common among women with sexual dysfunctions. In other words, it is not the parental divorce or absence of a parent per se that causes sexual dysfunctions, but the negative cognitions and attitudes that develop because of these conditions.
A majority of the patients were diagnosed with genito-pelvic pain/penetration disorder (81.5%), also known as vaginismus, followed by dyspareunia (8.6%), anorgasmia (6.2%), and absence of sexual desire (3.7%). We did not find a significant difference between the number or type of adversities and sexual disorder diagnoses. However, this was likely due to the small number of disorders other than genito-pelvic pain/penetration in the sample. Assessment of changes in sexual functions revealed that many patients reported problems with sexual desires as well as the ability to achieve sexual arousal and orgasm. An increase in the number of adversities was associated with problems in sexual arousal. A corollary finding was that more than half of the patients reported never engaging in cognitive activities or thoughts, such as sexual fantasies or the use of sexual media. This may arise from cultural conventions and expectations, or giving socially desirable responses, which warrants further investigation.
We did not find consistent associations between the number of adversities and increase in the occurrence of other medical conditions or disorders. In control participants, ACE scores were associated with having a higher number of medical diseases; however, in the patient group, this relationship was not significant. This stands in contrast to studies showing that adverse childhood experiences are associated with poor health status later in life. This may be the result of the sample’s younger age and the health care disparities in Armenia compared to other countries.
CONCLUSIONS
Two recommendations can be made on the basis of our study. The first recommendation is to raise awareness on the use of the ACE questionnaire, especially for professionals who assess and treat sexual disorders. Although the effects of childhood trauma on sexual dysfunctions are well known in the field, less is known about how other adversities, such as parental divorce or witnessing the mother being abused, can contribute to these problems as well. Also, childhood traumas, at least in Armenia, are often assessed inconsistently using unstructured methods, increasing the risk of failing to recognize the effects of childhood adversities on sexual disorder diagnoses. The ACE questionnaire, especially the Armenian translated version, can help Armenian speaking professionals as well as patients to be more informed about childhood adversities. The second recommendation is to develop and implement an ACEs Aware initiative in Armenia like the California ACEs Aware (2020) program. This California ACEs Aware program is led by the Office of the California Surgeon General and the Department of Health Care Services, which provide health professional training, clinical protocols, and payment for screening children and adults for ACEs. We are working toward implementing a similar program through a non-governmental organization that was co-founded by the first author. Our organization has provided various programs for medical and other health care professionals to promote sexual health and well-being. We plan to expand those initiatives to include programs that are specifically designed to screen and treat childhood traumas, using principles from single session therapy as a framework.


