BACKGROUND
In clinical practice there are many cases of children and adolescents who suffer from more than one mental disorder or developmental disorder (Kutscher et al., 2020). The symptoms may have different dynamics – they manifest mutually, occur simultaneously, overlap or mask, making an adequate diagnosis a highly difficult and complex task for the clinician (Lipowska, 2011; Winczura, 2012). The situation is also complicated by the fact that the manifestation of mental disorders’ symptoms in children is not a constant and homogeneous phenomenon. The clinical picture depends on many factors, concerning both the type of nosological syndrome and the specificity of a particular child’s development (Pisula, 2010).
The most common types of co-occurring disorders in children include autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), conduct disorders (CD), specific learning difficulties, anxiety disorders, obsessive-compulsive disorder, depression, bipolar disorder and others (Becker & Fogleman, 2020; Casanova et al., 2020; Munir, 2016).
Researchers report that autism has a strong tendency to co-occur with other disorders (BrookmanFrazee et al., 2018; Dizitzer et al., 2020; Mannion & Leader, 2016). The literature indicates that up to 70% of individuals with ASD have at least one cooccurring disorder and 40% of patients have two or more additional disorders (APA, 2013). The comorbidity between ASD and other disorders is of particular importance in child and adolescent clinical psychology. Understanding the contributing factors that interfere with the functioning of a young person with a multiple diagnosis helps to predict and eliminate developmental risk factors more accurately and to plan the appropriate therapeutic interventions as needed (Dizitzer et al., 2020).
The process of diagnosing a child with ASD and co-occurring disorders involves many observations in different contexts, taking an extensive diagnostic interview and using professional diagnostic tools (Winczura, 2018). An accurate diagnosis requires in-depth monitoring of the symptomology over a period of time to be certain of the correctness of conclusions (Lord & Luyster, 2006). It is therefore sensible to optimise the conditions of the diagnostic interventions – to have enough time to evaluate whether the diagnosis will be appropriate and not to prolong the process, causing significant disadvantages for the psychosocial development of the child. It seems extremely important to provide a full diagnosis early enough to implement an effective and more specific therapeutic intervention (Kirsch et al., 2020).
Therefore, the purpose of this article is to describe the age at which children with comorbid disorders begin the diagnostic process, the age at which they receive an ASD diagnosis, as well as the developmental and family-related environment factors that accelerate or delay the diagnostic process. In this regard, the paper also aims to point out the importance and necessity of improving parental awareness about the detection of early markers of disorders and to indicate aspects that minimise the risk of over-prolonging the diagnostic process. This study also aimed to investigate whether there is a difference in the age of diagnostic intervention and the age of ASD diagnosis between two groups of children diagnosed with comorbid disorders: ASD and externalizing disorders vs ASD and non-externalizing disorders.
FAMILY ENVIRONMENT, DEVELOPMENTAL AND OTHER FACTORS IN PSYCHOLOGICAL DIAGNOSIS OF CHILDREN
The diagnostic process begins much earlier than the first appointment with a specialist. The initial step, which brings a child closer to receiving a formal diagnosis, is the moment when parents or caregivers notice some developmental anomalies (BejaranoMartín et al., 2020; Mulligan et al., 2012; Steiner et al., 2012). Often a parent may notice alarming signs in the behaviour of child and then report it to a health professional – a general practitioner or psychologist. The caregiver is therefore the person who takes a crucial role by initiating the diagnosis and then implementing suitable steps in response to the opinion of an expert. The pre-diagnostic process aims at a preliminary recognition and a characterisation of the problems with which the individuals are struggling, so that in the next step they can receive help from a specialist (Kowalik & Brzeziński, 2000).
As the family is a privileged context for screening, previous research has shown that a parent may significantly reduce the duration of the diagnostic process by providing the clinician with complete and comprehensive information about the functioning of the child (McKenzie et al., 2015). Early detection of symptoms depends strongly on caregiver knowledge and awareness (Daniels & Mandell, 2014; Zablotsky et al., 2017). The quality of family life and level of stress correlate clearly with the length of the psychological diagnostic process (McKechanie et al., 2017). It is also worth noting that not everyone tends to seek professional help, especially if psychological services are not widely and easily available (Płatos & Pisula, 2019).
It is important to consider factors associated with the specific family system in which the child is raised, especially family stress factors. Undoubtedly, the system is influenced by both somatic diseases and mental disorders of the siblings and the parents of the child (Gulla, 2008). Children who have siblings with disabilities are faced with a situation that is emo-tionally challenging, with anxiety, anger, shame, guilt, and sadness (Twardowski, 2011). Having siblings with disabilities may also force one to face social rejection, reduced peer contact or adaptive difficulties (Marquis et al., 2019). Raising a child with a disability involves the need for greater parental availability and higher levels of stress. This may lead on one hand to overprotectiveness manifested in greater attentiveness to signs of disorders in siblings; and on the other hand, to idealize a child with a disability and ignore potential signs of disorders of another person (Boruszak & Gryglicka, 2014).
Research findings also indicate the relevance of some developmental indicators as predictors of early diagnosis (Rosenbaum & Gabrielsen, 2019; Rosenberg et al., 2011; Sicherman et al., 2021). An important factor is the cognitive functioning of children and their ability to perform adaptively in a social context (Bickel et al., 2015). Children with higher intelligence are diagnosed later than their peers with lower intellectual potential (Mazurek et al., 2014). The pace of intervention also depends on the severity of the symptoms of the disorder (Sheldrick et al., 2017). The parent or caregiver may therefore take some steps to identify the causes of alarming symptoms or fail to intervene. Factors related to the specificity of the family system and determinants related to the developmental path of the child are responsible for choosing the way to proceed.
There are also other relevant factors influencing psychological diagnosis of children which should be mentioned to get a more complex and complete picture of the problem. For example, family socioeconomic status significantly accelerates the process of diagnosis (Daniels & Mandell, 2014; Mazurek et al., 2014). The study of Mandell et al. (2005) showed that children who lives in urban areas received a diagnosis earlier than those living in rural areas. Additionally, a systematic review by Daniels and Mandell (2014) indicated that there is geographic variation in age of diagnosis. Family interactions with education and health systems before the diagnosis are also a predictive factor of age at diagnosis (Daniels & Mandell, 2014). Children whose paediatricians referred them to a specialist received a diagnosis earlier; on the other hand, children who had more than 4 primary care physicians received a diagnosis later (Mandell et al., 2005). Also school/nursery school context is important, especially when parents are not aware of the child’s symptoms and the teachers are.
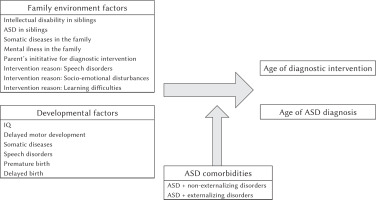
The authors of this research considered chosen family environment and developmental factors that form the background of the diagnostic process. These variables are presumed to have an important role in predicting the pace of specialist intervention for children with comorbid disorders.
Family environment factors in the diagnostic decision-making process are understood as conditions resulting from the upbringing of a child in a specific system which may be relevant to the reaction time to the symptoms of disorders. Family environment factors included:
intellectual disability of a sibling (IQ close to 70 or less, determined using selected intelligence tests),
ASD of a sibling,
somatic illness of a family member (physical illness, injury or physical disability),
mental illness of a family member (patterns of behaviours, ways of thinking, feeling, perceiving and other mental activities and relationships with other people, which are a source of suffering or difficulties in the individual functioning of the affected person),
initiating a diagnostic intervention at the initiative of a parent or caregiver (rather than at the suggestion of a teacher, social worker, or medical professional),
speech disorders as the main problem identified by the parent or caregiver (disrupted speech, e.g. speech impediment, delayed speech development as the main reason for diagnostic intervention),
socio-emotional disturbances as the main problem identified by the parent or caregiver (inadequate, disobedient, withdrawn behaviours of a child, difficulties in initiating and maintaining social relationship as the main reason for diagnostic intervention),
learning difficulties as the main problem identified by the parent or caregiver (problems in knowledge acquisition as the main reason for diagnostic intervention).
Developmental factors in the diagnostic decision-making process are included as conditions resulting from the course of development of a child. They might accelerate or delay the onset of symptoms of disorders:
intellectual capacity (IQ),
delayed motor development (problems with reaching developmental milestones in motor development),
co-occurrence of somatic diseases (disability),
co-occurrence of speech disorders,
premature birth (childbirth before 37th week of pregnancy),
delayed birth (childbirth after 40th week of pregnancy).
The above factors are considered to form the special conditions when the pre-diagnostic process happens. As in similar research projects such (or related) factors have been important in predicting the pace of the diagnostic process for developmental disorders (Mishaal et al., 2014), it is hypothesized that in the present study they may also have an impact on the comorbid disorder diagnostic process.
DIAGNOSTIC DECISION-MAKING IN CHILDREN WITH COMORBID DISORDERS
The process of diagnosing comorbid disorders in children and adolescents is an extremely complex and responsible task, requiring from the diagnostician both an extended knowledge of clinical psychology and the ability to apply it using their personal traits, such as diagnostic insight and curiosity, the ability to make contact with another person, to generate trust and to deal with possible resistance from the interviewee (Cierpiałkowska & Soroko, 2015; Winczura, 2012).
Although many children present symptoms at a very early age, they are diagnosed much later (Barbaro & Dissanayake, 2017). Most parents are not aware of a troubling behaviour until the second year of life (Skórczyńska, 2009). Some researchers report a long delay between noticing alarming signals and making a diagnosis (Christensen et al., 2018; Crane et al., 2016; Gray & Tonge, 2001). The age of ASD diagnosis varies from 3 to 12 years old (Daniels & Man-dell, 2014; May & Williams, 2018). It is speculated that the age of autism diagnosis may be even later if the diagnostician sees symptoms of other mental disorders in the clinical manifestations. The cooccurrence of other disorders may mask symptoms of autism or make the description of a child unclear. Delay in diagnosis has many negative consequences for the further development of the young person. A diagnosis of ASD before the age of 3 is optimal to implement effective therapeutic interventions (Ball, 2016; Dawson et al., 2012).
It therefore makes sense that the time is one of the most important determinants of the effectiveness in the diagnostic process. Early diagnostic and therapeutic interventions should be a priority in the treatment of mental disorders due to the greater vulnerability of the patient to compensate for deficits at a younger age (Angold & Egger, 2004; Schley et al., 2019).
In the context of ASD and other neurodevelop-mental disorders, a research area which has recently received significant amount of attention is early diagnosis. The increase in the number of studies in this area can be explained by the practical need to start therapeutic intervention as early as possible for the most effective results. Studies focus on behavioural markers identified within the first year of life using retrospective videotape analysis, high-risk infant siblings, genetic studies (to establish biological links), creating new tools; the aim is to form a system which efficiently screens and identifies children most at risk for developing ASD (Barbaro & Dissanayake, 2017; James & Smith, 2020; Matson et al., 2008; McCarty & Frye, 2020). As early detection by paediatric health-care providers is critical, activities also include programmes aimed at paediatricians and primary care physicians to facilitate the use of tools and adequate surveillance for autism so children can subsequently be referred for appropriate services.
The authors of this paper capture diagnostic decision-making, like Morrison and Flegel (2017), as the process of the clinician determining the diagnosis, leading to a judgment about the most appropriate diagnosis, which in practical terms means identifying a category that can be considered as the most likely (Morrison & Flegel, 2017).
The diagnostic decision-making process is operationalized in this research by referring to two key variables related to the time at which diagnostic choices are made: (1) the age of reporting a child for a diagnostic intervention – the first visit to a psychological and pedagogical counselling specialist, (2) the age of diagnosis of autism spectrum disorders as the most common co-occurring diagnosis in comorbid disorders. As the problem of the delayed diagnosis of the youngest is widely reported in contemporary literature (Daniels et al., 2014; Zwaigenbaum & Penner, 2018), it is considered that these variables would provide an illustration of the nature of the effectiveness of the diagnostic process of the group studied.
The primary aim of the study is to identify family and developmental predictors of the age of reporting a child for diagnostic intervention and the age of ASD diagnosis as the major disorder diagnosed in children with comorbid disorders. The second aim is to investigate whether there is a difference in the age of diagnostic intervention and the age of ASD diagnosis when the characteristic of comorbid disorder (externalizing vs non-externalizing) is taken into account.
The authors of the study decided to investigate the following research questions:
(1) What is the mean age of reporting for diagnostic intervention for children with comorbid disorders?
(2) What is the mean age of ASD diagnosis in children with comorbid disorders?
(3) What family and developmental factors are predictors of age of report for diagnostic intervention and age of ASD diagnosis in children with co-morbid disorders?
(4) Is there a difference in age of reporting for diagnostic intervention and age of ASD diagnosis between children with ASD and externalizing comorbid disorder and children with ASD and non- externalizing comorbid disorder?
This paper will provide an initial consideration of the specificity of diagnosing children and adolescents based on family environment and developmental background declared by the parent in the preliminary interview. The publication aims to highlight the aspects that may be most relevant in minimising the risk of prolonging the diagnostic process in children with comorbid disorders.
PARTICIPANTS AND PROCEDURE
STUDY DESIGN
The study procedure is based on a systematic, in-depth analysis of the documentation and treatment history of the patients of the public psychological and pedagogical counselling centres, including the medical opinion, the psychological testing results, the information from the clinical diagnostic interview and other important attachments. The data collection procedure consisted of directed scanning of patient files in order to obtain the necessary information among the overall documentatBoth children and their parents or caregivers provided permission for the interview and psychological testing, as evidenced by the appropriate documents in the individual patient files. The analysis of the research material was carried out between October 2020 and January 2021.
In this section it is worth mentioning how Polish psychological and pedagogical counselling centres work. Clarifying this issue is crucial for describing and understanding the nature of the data collected in the study.
The psychological and pedagogical counselling centres are the first point of psychological care for youth (from birth to the end of school education). The services are free of charge and widely accessible – every parent can register with a child in the local centre in the town of living or in the city where a child attends preschool or school.
The professionals in psychological and pedagogical counselling centres are qualified psychologists, pedagogues and speech therapists who have the specific expertise to support the decision-making process for the school system in Poland. However, an important fact is that they do not establish the diagnosis but assist the diagnostic process through initial monitoring of the pupils’ behaviour, conducting interviews and performing tests or observational scales. These specialists can refer patients to a medical doctor for a nosological diagnosis. Parents or caregivers are required to visit a qualified doctor themselves (public healthcare fund or private practice). After the appointment, they return to the specialist of the centre with information from the medical doctor about the diagnosis.
The diagnosis that will be mentioned in this paper is an effect of the decision of a medical doctor (usu-ally a psychiatrist) based on the diagnostic criteria of International Statistical Classification of Diseases and Related Health Problems (ICD-10), valid in Poland at that time. It is therefore believed that an opinion of a qualified medical doctor is sufficient proof of meeting the criteria for the disorder.
Thus, counselling centres are involved in mental health prevention, the initial identification of the problems of a patients, referring them to a clinician if necessary and, finally, therapy for children and support for parents, caregivers and teachers based on a diagnosis of a particular type of disorder. It is possible to trace individual cases and their medical history by using the data collected in the centre. The process of access to data on the medical history of the subjects was available since one of the authors was able to use the diagnostic files as a result of being a member worker at the psychological and pedagogical counselling centre. The researchers requested permission from the management of the counselling centre to analyse the data collected in the archives.
PARTICIPANTS
All Polish students identified with a disorder must visit the psychological and pedagogical counselling centre to receive recommendations for organising their education in accordance with their specific condition. School principals require guidance to provide the facilities for a pupil with special educational needs.
Given the specificity of counselling centres in Poland and their links to every school approved by the Ministry of Education, it is a highly heterogeneous group of visiting people. The cross-section of patients is varied in socio-economic status.
A preliminary analysis considered the documentation of all children who received an opinion about the need for special education in this psychological and pedagogical counselling centre due to the presence of any kind of disability in the school years 2018/2019, 2019/2020 and until January in the school year 2020/2021. Files were extracted if the participants met the specified criteria.
The inclusion criteria for the study are:
2-18 years old at the time of receiving a diagnosis of ASD,
having an opinion about the need for a special educational pathway provided by the Polish educational law,
access to the full educational history of a child,
the analysis of the documentation shows evidence that the child has been diagnosed with ASD and another disorder(s).
The exclusion criteria are listed below:
the child has been diagnosed with a single disorder,
lack of full documentation in the files of child, which makes it impossible to evaluate the reliability of details of the medical history.
Figure 1 illustrates how the analytic sample was defined.
Figure 1
Flowchart illustrating the definition of the analytic sample
Note. According to Polish educational law a person with multiple disabilities is a patient who has at least two of the following disorders: ASD, intellectual disability, sensory disturbances, hearing problems, vision problems.

Children have been diagnosed with co-occurring ASD and one or more of the following:
intellectual disability (31.30% of the children),
anxiety and/or depressive disorders (13.40% of the children),
specific learning difficulties (3.60% of the children),
sensory disturbances, i.e. motor disability, central auditory processing disorder, visual impairment, hearing impairment (29.50% of the children),
attention deficit disorders, disorganizing disorders and behaviours, such as ADHD, behavioural disorders, oppositional defiant disorders (46.40% of the children).
A quarter (24.10%) of the children were diagnosed with ASD and two comorbid disorders.
OUTCOME MEASURES
The following information about the children was collected during the analysis: gender, age, type of diagnosis, intelligence quotient, age of first reporting to the psychological and pedagogical counselling centre, age of receiving the ASD diagnosis, reason for first visit to a professional, the information about who brought the child in to be diagnosed, the information about the time of birth, existence of speech developmental delay and speech disorders, motor developmental delay, somatic diseases in the child, and psychiatric and somatic diseases in the family.
ETHICAL APPROVAL
Ethical review and approval were waived for this study due to the fact that data collected for educational purposes approved by the Polish Ministry of Education were used, in accordance with national procedures related to the testing of children in psychological and pedagogical counselling centre. The storage of these data respected the privacy of patients. These data can be used for statistical purposes.
STATISTICAL ANALYSIS
The authors of this research project predict that chosen family environment and developmental factors are significant for the age of diagnostic intervention and the age of ASD diagnosis in children with co-morbid disorders. The theoretical research model is presented in Figure 2.
Multiple regression tests were administered to analyse the data in R 4.0.5 software version. The ‘lm-test’ package was used for assessment of multivariate linear relationships (Hothorn et al., 2020).
RESULTS
STUDY POPULATION
Analysis of the full documentation of all children with a diagnosis of any kind of disorder allowed us to identify 112 patients who met the inclusion criteria. The individuals whose files were analysed were between 2 and 17 years old (M = 10.81, SD = 3.82). They were mainly boys (80.40%).
THE AVERAGE AGE OF DIAGNOSTIC INTERVENTION AND AGE OF ASD DIAGNOSIS
The mean age of first reporting for diagnostic intervention in the study group was 4 years and 3 months (M = 4.24, SD = 2.29). The age of receiving a diagnosis of ASD was 7 years and 3 months (M = 7.28, SD = 3.25). This implies that the study group typically had a lapse of about 3 years from the first visit to receiving a diagnosis of autism. The range for the age of diagnostic intervention is from 1 to 13, whereas the range of the age of ASD diagnosis is from 2 to 15.
THE CHOSEN PREDICTORS OF DIAGNOSTIC DECISION-MAKING
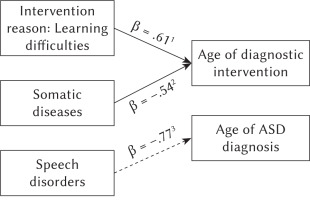
Two regression models were built predicting for age of diagnostic intervention and age of ASD diagnosis. The first omnibus regression model for the age of diagnostic intervention was significant F(14, 72) = 2.71, p = .008. Based on an adjusted R2 coefficient, tested variables in the regression model explained around 22% of variability of age of diagnostic intervention (R2 = .35, adj. R2 = .22). Analysis of the calculated model estimates showed that the somatic diseases were related to the earlier age of diagnostic intervention β = –.54, t = 2.09, p = .041, but learning difficulties as the reason for intervention was related to later age of diagnostic intervention β = .61, t = 2.09, p = .040. The analysis did not show any other significant relationships.
The second omnibus model for age of ASD diagnosis was insignificant F(14, 72) = 1.12, p = .074. Based on an adjusted R2 coefficient, tested variables in the regression model explained just around 2% variability of age of ASD diagnosis (R2 = .18, adj. R2 = .02). Despite the insignificance of the regression model, there was a result of borderline significance for speech disorders, β = –.77, t = 1.94, p = .056. This means that speech disorders were related to earlier age of ASD diagnosis. The analysis did not show any other significant relationships. All estimated results are presented in Table 1.
Table 1
The regression estimates in the tested models for age of diagnostic intervention and age of ASD diagnosis
The factors that were found to be significant in the diagnostic decision-making process are shown in Figure 3.
COMPARISON OF THE TWO GROUPS (EXTERNALIZING VS. NON-EXTERNALIZING COMORBID DISORDERS)
Children included in the study can be divided into two groups – those whose comorbid disorder is externalizing (attention deficit disorders, disorganizing disorders and behaviours, such as ADHD, behavioural disorders, oppositional defiant disorders) and those whose comorbid disorder is non-externalizing (intellectual disability, anxiety and depressive disorders, specific learning difficulties and sensory disturbances). The aim was to compare the age of diagnostic intervention and the age of ASD diagnosis in two groups of children diagnosed with comorbid disorders: ASD and externalizing disorders (n = 52) vs. ASD and non-externalizing disorders (n = 60).
Two t-tests showed that ASD comorbidities (as an independent variable) have an influence on the age of diagnostic intervention, t(109) = 1.99, p = .050, d = .24, but not on the age of ASD diagnosis, t(109) = 0.13, p = .083, d = .02. In the ASD and non-externalizing disorders group there was higher age of diagnostic intervention than in the ASD and externalizing disorders group, M = 4.71, SD = 2.40 vs. M = 3.85, SD = 2.14, but this effect was small (Cohen’s d = .24).
DISCUSSION
This study shows that the age of diagnostic intervention for children with comorbid disorders is around 4 years and it takes about three years to make a diagnosis of ASD. As a result, children receive an ASD diagnosis at the age of 7. This seems far too late for the therapeutic impact to be highly effective.
When comparing the results obtained with other studies on the same issue, one can see that the age is definitely later. An interesting comparison for this paper is the Australian research (Bent et al., 2020). In that study, it was found that parents report their child for diagnostic intervention at a mean age of 29 months (2 years and 5 months). Young patients receive an ASD diagnosis at an average age of 46 months (3 years and 10 months). Other publications also report much lower ages of ASD diagnosis, e.g. 2 years (Jayanath & Ozonoff, 2020) or 4 years (Berg et al., 2018). Hence, one may note that the age of ASD diagnosis revealed by the authors is frighteningly late.
The statistical analyses revealed that children are diagnosed with ASD at the age associated with the start of school education in Poland, although they have been under psychological care since early pre-school years. This phenomenon might be interpreted as a reluctance to refer to this diagnosis at earlier stages of development, in order not to follow the common tendency to overdiagnose children for ASD. However, when the demands of school environments arise, making a diagnosis of ASD can be considerably beneficial for the child who is underperforming in educational and social contexts. In our country the diagnosis of ASD implies many adaptations, which are guaranteed by education law based on an opinion from a public psychological and pedagogical counselling centre. The cost-benefit balance may be crucial in this context – diagnosticians make the decision to diagnose a child with ASD so as not to delay the development any longer or not to deprive the child of the chance to succeed in school.
Our results can be likened to the reports of researchers who point out that many children do not receive a diagnosis of autism until they start school (Brett et al., 2016).
It is worth emphasizing the fact that an earlier age of diagnosis enables the implementation of therapeutic interventions at a moment when the neuronal plasticity of the child is greater, and therefore the effects of interventions may be better. A later age of ASD diagnosis makes the chances for successful compensating for deficits limited (Kirsch et al., 2020; Schley et al., 2019).
The study provides an opportunity to indicate predictors of the early age of diagnostic intervention in children with comorbid disorders. The statistical analyses show that a significant predictor of the early age of reporting a child for diagnostic intervention is one of the developmental factors – the presence of a somatic disorder of the child. This association may result from the fact that the child has been under the medical care of a physician since early childhood, causing the environment to be more attentive in the evaluation of the developmental process. Somatic disease makes it compulsory to remain under the care of a specialist, which results in greater control over the regularity of psychophysical development and a greater chance to visit a psychologist due to observed problems. If the specialist notices alarming symptoms, he immediately suggests the parents visit a psychological-pedagogical counselling centre to deepen the diagnosis, so that the process of diagnostic decision-making starts when the child is very young.
The results also indicate that learning difficulties perceived by the caregiver are a predictor of an older age of reporting a child with comorbid disorders for diagnostic intervention. The pupils visiting the psychological and pedagogical counselling centre because of difficulties in learning material are brought to the psychologist late, which is probably connected with the detection of their difficulties at the stage of educational requirements. These children did not attract the attention of their caregivers earlier with other developmental difficulties (such as socio-emotional disturbances or speech disorders), so their diagnostic process begins when they experience educational failure. It therefore appears that the environment may be slower to recognize difficulties in the functioning of a child with comorbid disorders when their main concern is learning difficulties.
The statistical analyses also showed an effect that did not reach the adopted statistical significance level of .05, although it came close to meeting this criterion. It was discovered that speech disorders may be a predictor of early age of ASD diagnosis. The speech disorders may therefore accelerate the diagnosis of autism spectrum disorder in children with comorbid disorders. One of the axial symptoms of ASD is difficulty in communication development, which may attract the attention of the clinician immediately and suggest deepening the diagnosis to autistic disorder.
Our results correspond with the findings of similar research projects in which both developmental and family environment factors have been proven to be important in the diagnostic process. The severity of the symptoms, the developmental regression, having an older sibling (Mishaal et al., 2014), and IQ of the child were found to be significant predictors of the speed of the ASD diagnostic process (Mazurek et al., 2014).
Based on the data collected, the authors cannot make conclusion on other connections. Significance was found only for some of the studied factors. Thus, we cannot confirm the significance of other family environment factors tested (intellectual disability or ASD of siblings, somatic or psychiatric illness in the family, parental initiative for diagnostic intervention, speech or social-emotional disorders perceived by the parent) and developmental factors (IQ, motor developmental delay, somatic illness, premature or delayed birth). Future research may explore this topic in more depth and shed new light on the specifics of diagnostic decision-making in children with combined disorders.
Our results also show that there is a difference between the group of children diagnosed with ASD and non-externalizing comorbid disorder in age of diagnostic intervention (these children came to the specialist later than children with ASD and externalizing comorbid disorder). There was no difference in the age of ASD diagnosis in above-mentioned groups.
These results suggest that the specificity of the diagnostic situation of these two groups is different due to the different symptoms. Children diagnosed with ASD and externalizing disorders may have an earlier age of diagnostic intervention due to the fact that their behaviour is more unbearable to the environment and prompts parents to urgently seek help from professionals. Moreover, no difference in the age of ASD diagnosis in these two groups may indicate that problematic externalizing behaviour is understood as symptoms of other, similar disorders.
These findings encourage us to highlight the importance of the parental role in the process of psychological diagnosis of the child. Greater awareness of the specificity of the symptoms of the disorders has the potential to make it easier for family members to detect abnormalities in the development of the child even before beginning school when the learning difficulties are recognized.
Parental participation makes it possible to start the diagnostic process early enough to allow the diagnostic and corrective actions taken by professionals to have the most effective and quickest therapeutic results. Research shows that a proactive attitude of parents in the diagnostic process helps to make the diagnosis earlier (Zuckerman et al., 2015). Some results from studies show a significant discrepancy between parental perceptions of their involvement. The majority of parents feel totally or almost not involved in the interventions concerning the child, while the diagnosticians have the impression that almost three quarters of parents participate actively in the process (Bejarano-Martín et al., 2020). It would appear to be extremely important to establish an alliance between professionals and parents to improve the effectiveness of interventions for the child.
To the authors’ best knowledge, this is the first study in Poland which concerns the topic of family environment and developmental factors of diagnostic decision-making in children with comorbid disorders using data from a psychological and pedagogical counselling centre. The functioning of institutions which support the process of diagnosis is specific for each country. The systematic review by Daniels and Man-dell (2014) showed that the age in which diagnosis of ASD was made is different depending on the country the child lives in. This suggest that state policies, community resources and the way mental health institutions are operating play a role in early identification of ASD symptoms. This article gives an opportunity for reflection and comparison of the effectiveness and general functioning of this kind of institution in Poland and in other countries known to the reader.
Many studies focus on factors which are predictive in age of diagnosis of autism, but it is worth considering that there is an increasing number of children with comorbid disorders, such as ASD, ADHD, anxiety disorders, depressive disorders and others. Additionally, it is speculated that the age of autism diagnosis may be even later if the diagnostician sees symptoms of other mental disorders in the clinical manifestations, so the current study focused on children with comorbid disorders.
This article’s role is also to emphasize the role of mental health professionals in psychoeducation and raising awareness of neurodevelopmental disorders and basic marker symptoms of those, as well as information about proper development of a child among parents. An aware and attentive parent who can properly observe and detect abnormalities in the child’s development is the most important factor for early diagnosis.
Of course, the role of the school and the medical care context are also crucial and awareness-raising activities should also be undertaken there to create an effective system of screening and detecting the markers of disorders, so the diagnosis and, what is even more important, intervention can be implemented quickly. Future studies should focus on other than only family and developmental factors predictive in the age of diagnosis.
Examples of such activities in practice, aimed both at parents and education and health care professionals, include organizing training, courses and conferences to raise awareness of autism and other neurodevelop-mental disorder marker symptoms, creating practical materials such as brochures, articles, books, emphasizing the importance of observing the child in terms of achieving milestones in development, disseminating information about places and options for obtaining support, help and starting the diagnostic process.
LIMITATIONS
One of the limitations of the study is the inability to compare the results with data on the Polish epidemiology of combined disorders. There is a shortage of appropriate databases that provide information on prevalence. Statistics from psychological and pedagogical counselling centres do not include many co-morbid disorders as multiple disabilities, for example ASD and ADHD, ASD and anxiety disorders, ASD and dyslexia, ASD and many others.
Because official statistics are unavailable, it is impossible to judge whether the sample corresponds to the characteristics of the population of Polish children with comorbid disorders. There is a large data gap that makes it difficult to describe this group. There should be more detailed statistics conducted by the Ministry of Education. In the future, it is recommended that a similar study be carried out on a larger sample, including participants from different regions of Poland.
Another limitation is that 80.40% of the participants of this study were males. Although ASD is diagnosed more often among males, the proportion in the population is not so high as in our study and sex differences in ASD symptoms have been found in various studies (Hiller et al., 2014; Mandy et al., 2012; Rivet & Matson, 2011). Females have less impaired communication and social skills, and present less restricted interests and externalizing behaviours (Mandy et al., 2012; Rivet & Matson, 2011). Some studies have shown that ASD is diagnosed later in females than in males (Begeer et al., 2013). Taking those facts into account, it is possible that our results cannot be generalised to the girls and family and developmental factors which we found predictive are so only in males.
Psychological and pedagogical counselling centres are the first point of contact for parents who are concerned about the development of their child. These centres are generally accessible, free of charge and linked with preschools and schools in the region. The specialists of the counselling centres regularly visit local schools to observe children and offer appropriate assistance in case the initial analysis shows alarming signs. Therefore, it is very likely that parents and caregivers come to the counselling centre as a first point of contact with experts. However, one cannot eliminate the risk that there are also neglected children not attending schools or preschools, whose parents do not have the will to explain any developmental concerns. These children may live outside of the system because education is obligatory in Poland and failure to register in preschool and school results in harsh punishments for parents or taking the family under social assistance. The possibility of not capturing such people is present in all studies.
The researchers considered that the sampling of data from psychological and pedagogical counselling centres would be representative in view of the wide availability of these facilities in the community and the fact that specialists supervise every preschool and school accredited by the Polish Ministry of Education. However, it cannot be entirely dismissed that some Polish children may have been overlooked from this perspective.
CONCLUSIONS
The age of first diagnostic intervention for a child with a comorbid disorders is 4 years. The age of ASD diagnosis is 7 years. This age may be associated with the start of school education. Therapeutic interventions should be offered at a much younger age to be most helpful.
The chosen factors proved to be predictors of diagnostic decision-making in children with comorbid disorders. Among family environment factors, learning difficulties perceived by the parent or caregiver were found to be significant for delaying diagnostic intervention. Significant developmental factors include somatic illness, which accelerates the initial diagnostic intervention in children with comorbid disorders. The presence of a speech disorder may be relevant to the age of ASD diagnosis and may result in an earlier diagnosis, but this conclusion should be treated with considerable uncertainty.
There is a difference between the group of children diagnosed with ASD and non-externalizing comorbid disorder in age of diagnostic intervention (these children came to the specialist later than children with ASD and externalizing comorbid disorder). However, there is no difference in the age of ASD diagnosis in above-mentioned groups.
It is important to increase parental awareness of subtle symptoms of developmental disorders, besides learning difficulties. The earlier the first psychological consultation is made, the better the chances of an early diagnosis. Greater parental, but also medical care and education professionals awareness can bring many benefits to the diagnostic process.