BACKGROUND
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) differentiated trauma- and stressor-related disorders from anxiety and other fear-based symptom clusters (American Psychiatric Association, 2013). This differentiation should prove useful in emphasizing the unique and distinctive importance of trauma in the developmental trajectory of many health maladies. An important contribution of the DSM-5 task force was the generation of a precise and authoritative operational definition of “trauma” (Table 1, top panel). Trauma and its sequelae (flashbacks, heightened arousal, avoidance, and unwelcome cognitive and affective changes) constitute the basis for the post-traumatic stress disorder (PTSD) diagnosis. While a diagnostic advance, this operative conceptualization of trauma still involves subjective interpretations of criteria such as threatened death, serious injury, and sexual violation. This study examined the potential importance of perceived lifetime trauma as a risk indicator of self-reported health status.
Table 1
Trauma and PTSD symptomatology reported in the college and national samples
Patients with PTSD suffer from chronic medical illness and access primary health care at higher rates than counterparts without trauma exposure (Husarewycz et al., 2014; Sledjeski et al., 2008). Severe mental illness may mediate this relationship between PTSD and mental and physical health symptoms (Subica et al., 2012). Graded relationships have been found to remain even after rigorous controls for the potential influence of psychiatric contributors to these nexuses. One impressive national cross-sectional analysis (Husarewycz et al., 2014) of face-to-face structured interviews conducted by lay census workers (N = 34,653) found significant adjusted effect sizes for links between lifetime injurious trauma and cardiovascular disease (OR = 1.41, p < .001), diabetes (OR = 1.45, p < .001), arteriosclerosis/hypertension (OR = 1.16, p < .001), obesity (OR = 1.14, p < .001), gastrointestinal illness (OR = 1.22, p < .01), and arthritis (OR = 1.45, p < .001). This study relied instead on anonymous crowdsourcing self-reports of trauma and health status with attempts to also control variance associated with PTSD and other psychiatric diagnoses.
Childhood adversity is a broad term applied to circumstances that include maltreatment (sexual abuse, physical abuse, and emotional abuse), neglect (physical and emotional), and a range of household stressors (e.g., parental divorce, intimate partner violence, parental alcoholism, family mental illness, sibling incarceration). Severe forms of childhood maltreatment can meet the operational criteria for trauma described in the DSM-5. Adults with more extensive medical histories often report exposure to adverse childhood experiences (ACEs) at a disproportionate rate to that of healthier counterparts (Anda et al., 2006; Dong et al., 2003, 2004; Dube et al., 2002, 2003; Felitti et al., 1998; Hillis et al., 2000, 2001, 2004).
Patients with a higher ACE count exhibited elevated (60%) risk for diabetes as adults (Felitti et al., 1998; Rich-Edwards et al., 2010). Type 2 diabetes rates were higher among women recalling unwanted sexual touching (16%) or either isolated (34%), or recurrent (69%), child or adolescent sexual assault than non-abused counterparts (Rich-Edwards et al., 2010). Diabetes rates were elevated among patients with histories of childhood neglect (Goodwin & Stein, 2004; Rich-Edwards et al., 2010; Shaw & Krause, 2002). ACE counts have been associated with functional somatic syndrome that includes fibromyalgia, chronic fatigue, and irritable bowel syndrome (Afari et al., 2014). ACEs may lead to poorer health via activation of magnified stress responses early in life (Lindert et al., 2014). ACE stressors may even alter gene expression and accelerate aging (Lang et al., 2020). Evidence for trauma-health nexuses has been equivocal. A study from the Netherlands found links between somatic and psychiatric disorders (e.g., PTSD, depression, anxiety disturbance), but not specifically adverse life experiences (van der Feltz-Cornelis, 2019). Other analyses have found the attenuation of these trauma-health links after covariate (e.g., PTSD, generalized anxiety, smoking and drinking histories, other demographics) adjustments (Keyes et al., 2013).
Psychiatric illnesses other than PTSD have also been associated with physical illness. Anxiety disorders were linked to an increased risk of medical illnesses and associated treatment complications (Asmundson & Katz, 2009). Chronic arthritic pain was higher among anxious versus non-anxious patients in a community sample (Kessler et al., 2003). Irritable bowel syndrome (IBS) symptomology was also higher among patients with an anxiety disorder (Sykes et al., 2003), while visceral hyperalgesia seemed to be induced or aggravated by stress and anxiety (Mayer et al., 2001). The prevalence of autoimmune disease (e.g., celiac disease, rheumatoid arthritis) appears higher among patients with psychotic disorders (Jeppesen & Benros, 2019).
The immunosuppressant effects of stress may account partially for associations between trauma and health. T-cell, leukocyte, and lymphocyte counts were found to be higher among military veterans with PTSD (Lauterbach et al., 2005). More than half of military veterans with PTSD in one outpatient sample reported chronic pain (Asmundson & Katz, 2009). Childhood trauma appears to magnify inflammatory processes at a molecular level while increasing victim susceptibility to both psychiatric and physical illnesses (Baumeister et al., 2016). Childhood maltreatment survivors have been shown to be encumbered by higher EEG-derived cognitive workloads during executive functioning tasks than non-abused counterparts (Mark et al., 2019). Cicchetti (2016) posited that early traumas may disrupt hierarchical, age-related, formative tasks including parental bonding, affective control, self-image formation, peer relations, and other critical landmarks. Biosocial researchers hypothesize that developmental insults alter the neural substrates that mediate emotional expressiveness (Cicchetti, 2016; Cicchetti & Rogosch, 2001; Kim et al., 2009). Personality traits provide natural mechanisms for the translation of early trauma into adult psychiatric symptomatology (Oshri et al., 2013; Spinhoven et al., 2016).
Disproportionate attention has been placed on pathologic outcomes of trauma and adversity in the psychiatric community. A different line of evidence re-emphasizes that maladjustment is not always the outcome of lifetime adversity and trauma. Feelings of grief and depression often diminish over time with the trauma serving as a catalyst for growth, confidence, self-reliance, and other adaptive outcomes (Andriessen et al., 2018; Michael & Cooper, 2013; Ogińska-Bulik, 2018; Rahmandani et al., 2022; Schwartz et al., 2018). The resiliency literature informs the trauma research and practice communities that lifestyle improvements can accompany the psychological changes imposed on victims of trauma.
HYPOTHESES
Analyses were designed to estimate the strength of the association between trauma exposure and perceived health status. Three broad hypotheses were examined: H1) lifetime medical diagnoses would be more prevalent among respondents with self-reported trauma exposure; H2) these trauma-health relationships would be stronger among respondents who described PTSD symptomatology; H3) trauma-health associations would remain significant even among respondents who denied past psychiatric illness.
PARTICIPANTS AND PROCEDURE
PARTICIPANTS
This study examined convenience archival college (n = 2,320) and national (n = 663) samples. The college respondents were compensated with course extra credit. MTurk respondents were paid 40 cents. The survey was accessed through either the SONA Systems or MTurk research platform. This project was IRB-approved (IRB-201905-301; IRB-201903-238) with informed consent required for all respondents. Respondents in this study contributed to one earlier analysis of different criterion measures (King et al., 2019). The college sample was represented by respondents of varying gender (75.7% women, 24.1% men), age (M = 20.12, SD = 3.98, range = 18-55), and ethnicity (White 89.4%, African-American 2.2%, Hispanic 1.6%, Asian 1.9%, American Indian 1.9%, and Multi-Racial 3.0%). The national sample was represented by respondents of varying gender (43.9% women, 56.1% men), age (M = 38.10, SD = 12.19, range = 18-78) and ethnicity (White 75.8%, African-American 8.8%, Hispanic 5.3%, Asian 5.6%, American Indian 1.8%, and Multi-Racial 2.7%). Analyses were not conducted on additional college (n = 324, 12.2%) and national (n = 306, 31.6%) subsets that failed to meet the inclusion and exclusion criteria specified below.
INCLUSION CRITERION
Respondents were not included in the analyses (college, n = 193; national, n = 102) if they failed to complete either the trauma or medical diagnosis panels.
EXCLUSION CRITERIA
This analysis relied on self-reported medical diagnoses for up to 19 different health maladies. The initial distributions of self-reported diagnoses within the college (M = 1.03, SD = 1.29, range = 0-19, skewness = 3.27) and national (M = 2.20, SD = 3.96, range = 0-19, skewness = 3.15) samples were skewed with small subsets tending to have disproportionate numbers of diagnoses. Best-practice recommendations (Aquinis et al., 2013) were followed to exclude those outliers with scores above or below 2.24 standard deviations from the college (> 5 diagnoses, n = 18) and national (> 11 diagnoses, n = 35) distribution means.
Respondent subsets were excluded due to a report of: (a) symptoms of a traumatic experience that was not identified (college, n = 101; national, n = 55); or (b) a PTSD diagnosis without identification of a past trauma (college, n = 12; national, n = 7).
Amazon’s Mechanical Turk (MTurk) was used to generate this crowdsourced sample. MTurk has been reviewed favorably as a crowdsourcing research platform (Buhrmester et al., 2011; Gosling et al., 2004; Paolucci et al., 2001). A concern regarding crowdsourcing methodology has been raised regarding the potential threat posed by international bot farms that disguise their origination (Kennedy et al., 2020; Moss & Litman, 2018). This MTurk sample was restricted to respondents of at least 18 years of age who completed the survey from the United States. Online proxy/VPN detection software (https://iphub.info) was relied upon as recommended (Burleigh et al., 2018) to identify and exclude initial respondents (n = 12) who attempted to disguise their international origin. Additional precautions were taken to exclude respondents who failed an English language reading verification (n = 1), missed an attention check item (n = 7), or completed the survey from a duplicated internet provider address (n = 9) or geolocation (n = 48).
ASSESSMENT
Trauma history assessment. The trauma history panel (Table 1, top panel) was worded to match the primary DSM-5 diagnostic criterion for post-traumatic stress disorder (American Psychiatric Association, 2013). Trauma history was classified into two cells (no trauma, n = 1,922; trauma reported, n = 360). A trauma exposure group was also formed to differentiate symptomatic from non-symptomatic trauma histories (no trauma, n = 2,294; trauma without PTSD, n = 566; trauma with PTSD, n = 123). While the reliability of self-identified trauma has not been established, self-reports of adversity exposures appear fairly stable over time. Face valid single-item data have been relied upon in selected behavioral science studies (Allen et al., 2022). Retrospective reports of general childhood maltreatment were found to be reliable (r = .50) among young adults (N = 980) in a longitudinal analysis tested at ages 18 and 21 (Fergusson et al., 2011). A sample of medical patients (N = 608) was retested on the ACE Questionnaire in a 20-month follow-up (Dube et al., 2004). The total ACE count (κ = .64, 95% CI [.61; .77]) and individual item kappas showed moderate to good reliability for sexual abuse (κ = .69, 95% CI [.61; .77]), physical abuse (κ = .55, 95% CI [.47; .63]), emotional abuse (κ = .66, 95% CI [.55; .76]), and exposure to intimate partner violence (κ = .77, 95% CI [.68; .85]). Estimates did not vary markedly by age, sex or education.
Medical diagnoses (MedDiags). The selected diagnosis clusters were designed to canvass respondents about a representative list of common conditions. The medical diagnosis panel asked respondents about past “health concerns”: “Have you been diagnosed with any of the following medical conditions (leave item blank if answer is no or item is not applicable)?” A total of 19 health conditions were selected for inclusion in this analysis after reviewing the common non-psychiatric diagnoses (Rowley, 2011; Sauver et al., 2013). The accuracy of self-reported medical diagnoses within a large (N = 43,000) Canadian public health research platform appeared to vary as a function of the diagnosis (Payette et al., 2020). Kappa coefficients range from excellent (κ > .60 for hypertension, diabetes, cardiovascular disease, and breast/prostate/thyroid/bladder/lung/kidney cancer) to moderate (κ > .40 for asthma, and epilepsy) to poor (κ < .40 for irritable bowel syndrome and rheumatoid arthritis). MedDiags was a criterion variable calculated as the total number of medical diagnoses identified by each respondent. The exact wordings for these medical conditions were intended to be general and comprehensible within the general public: cancer or tumor (malignant), heart disease, hypertension, concussions (multiple), migraine headaches, seizures, chronic back pain, fibromyalgia, HIV/AIDS, diabetes, asthma, arthritis, ulcer, irritable bowel syndrome, acne, liver damage or disease, kidney stones, and/or bed wetting in childhood.
Psychiatric diagnoses (PsyDiags). Traumatized respondents were differentiated in selected analyses by whether or not they reported a prior PTSD diagnosis. A psychiatric diagnosis panel canvassed respondents about common DSM-5 (American Psychiatric Association, 2013) disorders including (exact wording): drug addiction, alcohol addiction, attention deficit hyperactivity disorder, bipolar disorder, borderline personality, major depression, schizophrenia, panic attacks, post-traumatic stress disorder, obsessive-compulsive disorder, learning disability (any), and/or bulimia or anorexia nervosa. A subset (n = 131) of the present college archive was retested (two week average) during initial data collection to establish the temporal stability (κ = .83, SE = .10) of their self-reported diagnostic histories of post-traumatic stress disorder.
Perceived physical health status (vitality). Respondents were asked to provide a self-assessment of their own health using the following question: “On the scale below how would you rate your current physical health?” Anchor descriptions were provided for the lowest (poor health) and highest (excellent health) poles of the ten-point continuum.
Results
DESCRIPTIVE STATISTICS
Prevalence rates for self-reported trauma (Table 1, bottom panel) differed in the college (17.5%) and national (42.5%) samples, χ2(1) = 181.30, p < .001. Trauma prevalence varied by gender in the college sample (women, n = 329, 18.7%; men, n = 77, 13.8%), χ2(1) = 7.19, p = .007. Gender differences were not found in the MTurk sample (women, n = 169, 45.4%; men, n = 113, 38%), χ2(1) = 2.91, p = .088.
Symptom endorsements were counted for respondents who identified past trauma. The number of symptom clusters identified by traumatized respondents (0 symptoms, n = 107, 26.3%; 1 symptom, n = 66, 16.2%; 2 symptoms, n = 65, 16.0%; 3 symptoms, n = 62, 15.2%; 4 symptoms, n = 107, 26.3%) did not differ by gender in the college sample, χ2(4) = 7.91 p = .095. The number of symptom clusters identified by traumatized respondents (0 symptoms, n = 53, 18.8%; 1 symptom, n = 39, 13.8%; 2 symptoms, n = 39, 13.8%; 3 symptoms, n = 24, 8.5%; 4 symptoms, n = 127, 45.0%) did not differ by gender in the MTurk sample, χ2(4) = 2.87, p = .580.
Table 2 documents frequency distributions for the medical (MedDiags) and mental health (PsyDiags) diagnostic counts. Respondents were selective in their affirmations of prior diagnosed medical (89.9%, two or less) and psychiatric (96.9%, two or less) illness.
Table 2
College (N = 2,320) and national (N = 663) sample distributions
[i] Note. MedDiags options included cancer, hypertension, migraine headaches, diabetes, asthma, ulcer, irritable bowel, kidney stones, liver disease, multiple concussions, heart disease, seizure disorder, chronic back pain, fibromyalgia, arthritis, HIV/AIDS, acne, and/ or enuresis. PsyDiags options included post-traumatic stress disorder, alcohol addiction, drug addiction, panic disorder, obsessive-compulsive disorder, major depression, bipolar disorder, borderline personality disorder, schizophrenia, attention deficit/hyperactivity disorder, learning disability, and/or bulimia or anorexia nervosa.
Table 3 shows differences between the observed (MTurk sample) and adult United States illness prevalence estimates using observer-expected single sample proportion tests (Fleiss et al., 2003). MTurk prevalence rates were equal (liver disease, heart disease, enuresis, HIV/AIDS, chronic back pain, and multiple concussions) or significantly lower (cancer, hypertension, diabetes, kidney stones, ulcer, irritable bowel syndrome, arthritis, fibromyalgia, and acne) than population estimates. Three illnesses (migraine headaches, asthma, and fibromyalgia) were more prevalent in the MTurk sample. National prevalence estimates in this analysis were consistent with those found in the MTurk sample (r = .76, p < .001).
Table 3
Current sample and United States adult medical diagnosis prevalence rates
[i] Note. Sample frequency count (prevalence). Current epidemiology estimates for United States adult prevalence rates were derived from the following sources: aCenters for Disease Control and Prevention (CDC); bLovell & Ford, 2012; cScales et al., 2012; dVeliz et al., 2017; eShmagel et al., 2016; fBickers et al., 2006; gAmerican Psychiatric Association, 2013. Bolded national prevalence estimates differed significantly from the MTurk sample rates. National and MTurk prevalence estimates were significantly associated (r = .76, p < .001).
ANALYSES OF COVARIANCE
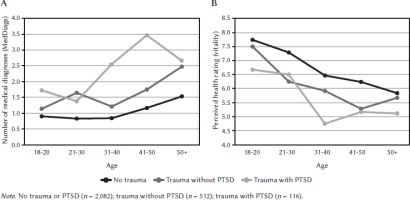
Analyses of covariance (Table 4) were used to assess effects of age, sample, gender, and trauma exposure on medical diagnoses (MedDiags) and perceived physical health status (vitality). Trauma exposure effects were significant for both criterion measures, and vitality differences were larger within the MTurk as opposed to the college sample.
Table 4
Health status indicators as a function of sample, gender, and trauma exposure
Trauma exposure results for MedDiags (Figure 1A) were as follows: trauma with PTSD (n = 116, M = 2.15, SD = 1.81); trauma without PTSD (n = 512, M = 1.44, SD = 1.64); no trauma (n = 2,082, M = .91, SD = 1.10). Significant differences (p < .001) were found for MedDiags between all three conditions: trauma without PTSD > no trauma or PTSD (d = .46. p < .001); trauma with PTSD > no trauma or PTSD (d = .83, p < .001); and trauma with PTSD > trauma without PTSD (d = .38, p = .020).
Trauma exposure results for vitality (Figure 1B) were as follows: trauma with PTSD (n = 116, M = 5.87, SD = 2.14); trauma without PTSD (n = 512, M = 6.56, SD = 2.02); no trauma (n = 2,081, M = 7.44, SD = 1.69). Significant differences were found for vitality across all three conditions: trauma without PTSD > no trauma or PTSD (d = .41); trauma with PTSD > no trauma or PTSD (d = .96); and trauma with PTSD > trauma without PTSD (d = .55).
CATEGORICAL AND RELATIVE RISK ANALYSES
Significant prevalence differences were found between the control (no trauma or PTSD) and trauma alone (no PTSD) condition for 14 of the 18 medical diagnoses (Table 5). Relative risk estimates from the contrast of trauma and no trauma conditions (no PTSD reported within either cell) ranged to a high of 5.53 for fibromyalgia. Significant differences were still found in 7 of 18 diagnoses even after control of the impact of a prior psychiatric history (see Table 6).
Table 5
Frequency differences in total sample of medical condition by trauma exposure
Table 6
Illness prevalences in sample subset with no psychiatric diagnoses (n = 2,282)
Discussion
Trauma is a word used historically in professional and public circles to describe disturbing life events. Clinicians and researchers now rely on the operational definition of trauma provided by the DSM-5. This study examined the extent to which survey respondents would identify trauma exposure as defined by this authoritative source (e.g., life events that involved actual or threatened death, serious injury, or sexual violation of self or other). Self-reports of trauma were found to be common in college (17.5%) and national (42.5%) samples. An important question remains as to the clinical significance of perceived trauma on both mental and physical health status with or without associated psychiatric disturbance. Trauma, adversity, and child abuse have been identified widely as risk indicators for many different forms of psychiatric and other medical illness. This study examined health correlates of self-identified lifetime trauma using a standard DSM-5 operational definition.
Significant associations between self-reported trauma and physical health status were found to remain even after control of variance associated with PTSD and other psychiatric diagnoses. Endorsements of this single DSM-5 criterion had risk implications for a range of broadly defined medical conditions. Relative risk estimates for these various medical diagnoses appeared consistent with the largest and most rigorous national survey to date regarding trauma and health (Husarewycz et al., 2014). All three hypotheses were supported: (H1) Self-identified trauma was associated with higher prevalence rates for 16 of 18 medical diagnoses; (H2) PTSD diagnoses were associated with higher prevalence rates than trauma alone for 6 of 16 medical conditions; and (H3) self-reported trauma was associated with higher prevalence rates for 7 of 18 medical conditions among respondents who denied psychiatric histories.
LIMITATIONS
These trauma-health associations must be qualified with interpretive cautions. This was an uncontrolled cross-sectional analysis with causation and directionality not established. The timings of the trauma and health correlates were not identified. The onset of severe medical illness itself could have constituted the trauma described by selected respondents. Traumas described by selected respondents may have led directly to selected medical conditions such as concussions, seizures, or back pain. Inattentive responding likely inflated predictor and criterion scores for some respondents. “Cries for help” among stress-ridden respondents may have led to overreporting of both trauma and illness. The validity of even conscientious self-reports can be challenged within subsets of the samples.
While inattentive or indiscriminate responding is a concern in every survey analysis, inclusion and exclusion criteria were implemented to minimize these sources of error variance. Diagnostic endorsements appeared to be discriminating for most respondents who identified a narrow subset of panel options. MTurk prevalence rates exceeded population estimates for only three illnesses. Endorsement rates otherwise approximated or underestimated epidemiologic sources (Table 3). Diagnoses thought to be most vulnerable to stress-related exacerbation (e.g., migraines, hypertension, irritable bowel syndrome, fibromyalgia, back pain) generated the highest odds ratios in this analysis (Table 5). Empirical support can be found for the general accuracy of self-reported health (Payette et al., 2020) and maltreatment (Dube et al., 2004; Fergusson et al., 2011) histories. PTSD diagnoses were found in this college sample to be consistent across retesting. Medical providers routinely rely on patient self-reports from intake through treatment. Face valid single-item data have been relied upon in selected behavioral science studies (Allen et al., 2022).
IMPLICATIONS
Associations identified in this article involved perceptions of trauma and health with room for both direct (physiological) and indirect (psychological) risk contributions. Traumatic experiences can directly impact physiological functions (Baumeister et al., 2016; Cicchetti, 2016; Cicchetti & Rogosch, 2001; Kim et al., 2009; Lauterbach et al., 2005), and ample evidence points to the broader impact of PTSD symptomatology as a physical health risk (Asmundson & Katz, 2009; Mark et al., 2019; Oshri et al., 2013; Spinhoven et al., 2016). ACE exposures have been linked to both physical (Felitti et al., 1998) and psychiatric (Anda et al., 2006) symptomatology, and trauma constitutes an extension of adversity research. It is important to recognize the complexity of these links between formative life experiences and distal health that can deteriorate in different slopes over time. Early life trauma could trigger lifestyle changes that require a long course to impact health. Efforts to identify bio-stress mechanisms (Lang et al., 2020; Lindert et al., 2014) that somaticize trauma exposure are essential to the advancement of current understanding of these complex nexuses. Even in those cases where mental and physical health deteriorate independently, concerns in one risk domain should draw closer attention to all aspects of functioning. In lieu of precise prognostic standards regarding traumatic exposure, practitioners should recognize the potential significance of self-identified trauma and the range of potential biosocial implications that may warrant monitoring.