BACKGROUND
PARENTING A PREMATURE BABY
The duration of a normal pregnancy is expected to be anywhere from 37 to 40 weeks of gestation, and the World Health Organization defines babies born before 37 weeks as preterm. More than 1 in 10 babies in the world, adding up to approximately 15 million babies a year, are born preterm, and their families are affected (Howson et al., 2013). Moreover, as Blencowe et al. (2012) reported, over 1 million babies die due to complications caused by preterm birth.
Preterm infants need to be cared for in a neonatal intensive care unit (NICU), with the duration determined by the babies’ condition. The more preterm and/or low weight an infant is at birth, the longer the infant needs to spend in the NICU, which also poses increased health risks. Being preterm can cause many lifelong problems for an infant from birth or in the NICU. Serious health problems and physical or mental barriers that may occur can impose heavy burdens on both the baby and the family that make life harder. In preterm birth, for every week a baby is born before the 38th gestational week, the risk of morbidity doubles (Shapiro-Mendoza et al., 2008). Whereas infants born at 24 weeks have a 50% chance of survival in high-income countries, the same rate applies only to those born at 34 weeks or older in low- and middle-income countries (Blencowe et al., 2012).
Under the difficult circumstances they face, parents who have preterm babies are subject to many stressors. The addition of a baby to the family is usually a happy event for families. However, in some circumstances, such as preterm birth or a birth with complications, it manifests as a traumatic event that poses a major stressor for the family and has the potential of affecting family dynamics. Ideally, birth is a magical experience of the mother uniting with the baby after months of anticipation during pregnancy; however, when a child is premature, the mother and baby must often be separated immediately after birth to administer neonatal care to the baby. Thus, the birth experience becomes traumatic, regardless of whether the threat of preterm birth was previously known to the parents (Affleck & Tennen, 1991).
The second stressful period for parents of preterm infants starts immediately after the baby is discharged and taken home. Goldberg (1978) noted that the postdischarge care of preterm infants is much more difficult than that of term infants; preterm infants need to go to the hospital more often because of allergies, ear infections, and other health-related causes. Compared with parents of term infants, parents of preterm infants have to wait longer to see positive indicators of growth and development, such as laughing, motor development, and uninterrupted sleep. Thus, their stress persists for a long time, even after discharge (Goldberg, 1978). The first year of life of preterm infants is more difficult than it is for term infants, and parents must cope with greater physical, emotional, and financial burdens (Okumus, 2012).
Miles and Holditch-Davis (1997) suggested that parents of infants hospitalized in the NICU – especially mothers – have intense emotional responses. A synthesis of the findings from the descriptive studies reports that anxiety, helplessness and loss of control, and fear, as well as guilt and shame, depression and sadness, and a sense of failure and disappointment are the most typical feelings parents experience. Although studies indicate that extreme anxiety of parents decreases over time, parents still have worries and related anxiety when the infant is discharged home for care (Leahy-Warren et al., 2020; Treyvaud et al., 2019).
Schappin et al. (2013) reported that the stress levels of parents of preterm and term infants do not differ significantly. However, stress levels of parents vary depending on preterm infants’ health characteristics, such as birth weight: the greater the birth weight, the smaller the difference. This may be because lower birth weight is associated with higher levels of infant morbidity and mortality (Shapiro-Mendoza et al., 2008).
Treyvaud et al. (2019) stated that preterm birth and admission to the NICU is a distressing and potentially traumatic experience for the parents. Their study suggested that parents need individual psychological and psychosocial support, peer-to-peer support, and broader early intervention programs to maintain and develop their wellbeing, including mental health. Parents, especially mothers, show symptoms of trauma following the preterm birth of their infant. Some suffer from psychological trauma even for a longer period after hospital discharge (Jotzo & Poets, 2005). In their study, Leahy-Warren et al. (2020) observed that mothers of preterm infants are at a 38% higher risk of postpartum depression within the first year after NICU discharge. Not surprisingly, the results of the study also show that having a high level of functional support is associated with a lower level of depressive symptoms.
THE PSYCHOLOGICAL IMPACT OF PARENTING A PREMATURE BABY AND RELATIONSHIP DYNAMICS
Partners’ deepest needs for close human connections are addressed in a romantic relationship. Romantic relationships are the source of emotional dependency on the partner. Emotional dependency can be defined as a person’s attachment to the partner in a relationship and the importance of the relationship with the partner compared with other alternatives and things in life (Buunk, 1982, 1995). Kemer et al. (2016) found that emotional dependency is the major predictor of relationship satisfaction among Turkish partners. This may be an expected positive outcome, considering the importance of humans’ fundamental needs, such as being loved, connection with others, and intimacy. Robinson and Blanton (1993) included ‘interdependence’ in intimacy, which they defined as one of the characteristics of enduring marriages. Studies show that dependency is related to greater adjustment (Cirhinlioğlu et al., 2017; Rusbult & Verette, 1991; Rusbult et al., 1991), relationship satisfaction (Erol & Orth, 2013; Rusbult et al., 1991) better self esteem (Erol & Orth, 2013; Robinson & Cameron, 2012) in couples. In their study with 466 married individuals, Cirhinlioğlu et al. (2017) found that emotional dependency leads to better adjustment between partners, more effective communication, and more effective problem solving in the relationship.
Relationship quality is multidimensional and can be described using multiple terms, including relationship satisfaction, commitment, intimacy, affection, and understanding (Farooqi, 2014). We think that Kelley and Thibaut’s (1978) interdependence theory offers a noteworthy explanation for satisfaction, dependence, and commitment in dyadic relationships. They note that interaction between partners is the essence of all intimate relationships. The theory suggests that satisfaction level and degree of dependence are two important components of an ongoing relationship. The investment model asserts that the state of dependence relates to feelings of commitment, where the commitment level is a psychological state that reflects the overall experience of dependence on a relationship. Rusbult and Buunk (1993) argued that the commitment level reflects the effects of other dependence-enhancing variables, such as satisfaction, alternatives, and investments. Highly committed individuals need to connect to their partners, and the satisfaction level affects the commitment level. Thus, individuals’ level of commitment directly affects their dependence on their partner and the decision to terminate or remain in the relationship (Rusbult & Buunk, 1993).
Stress is the state of emotion felt when problems that people need to deal with challenge their physical and psychological health and exceed their skills and available resources. All situations that require adaptation can be regarded as potential stressors. Stressors are external requirements that cause emotional disturbance; their effects on the organism are defined as stress, and the actions that are used for managing the stress are called coping mechanisms (Butcher et al., 2013).
According to Lazarus and Cohen (1977), in the study of stress, researchers in various disciplines have observed that stress has three features, and each of these features has attracted significant research attention. First, the emotion and effects of stress have a major effect on satisfaction and morale. Second, stress affects individuals’ adaptation skills, such as problem solving, social coherence, and somatic health. Finally, when such emotions as anxiety, fear, guilt, resentment, sadness, or anger arise as a result of stress, their presence reveals that significant psychological events are taking place between individuals and their environments. The factors that indicate the potential level of influence of a stressor are defined by its severity, whether it is ongoing, the timing, how closely it affects the person’s life, and how predictable and controllable it is (Butcher et al., 2013).
Depression is a state of deep dejection in which the individual feels severe sadness and despondency. It is often accompanied by impairment of thought, speech, psychomotor and physiological functions, and stagnation. It is also a syndrome characterized by feelings and thoughts of worthlessness, weakness, powerlessness, and pessimism (Ozturk & Ulusahin, 2016). Perinatal depression describes depression experienced during pregnancy and within the first year after birth. Predisposition to mental illness increases the most in the perinatal period, and there are various biological and psychosocial factors affecting it. Low socioeconomic status, history of depression in an immediate family member, problems with the partner, a high-risk pregnancy, and a history of previous postpartum depression are some risk factors for perinatal depression (Ozturk & Aydin, 2017).
Postpartum depression affects around 10-15% of mothers and is one of the most important complications of giving birth (O’Hara & Swain, 1996). Although family history is considered for depression, some stressful experiences also increase the risk of postpartum depression (Vigod et al., 2010). In Vigod et al.’s (2010) review study, four studies out of six showed that the frequency of depression of the mothers of preterm infants was significantly higher, especially in the first year after birth, compared with mothers of term infants. The study also showed that mothers of preterm infants have a 1.6-fold increased risk of depression within the first 8 weeks after birth.
A study from Australia reported that 40% of 62 mothers who gave birth to preterm infants between the 24th and 32nd gestational weeks showed symptoms of depression (Davis et al., 2003). The main source of these symptoms was revealed to be maternal stress. It is clear that factors such as being separated from their small babies, who are facing many health risks and are even at risk of death; not being the primary caregiver; and spending time with their babies for only a limited time increase mothers’ stress.
Preterm birth and maternal or fetal health problems that lead to it are also sources of stress. Ideally, a new mother will be healthy, and this will have a positive impact on the couple’s relationship. However, if the pregnancy or birth is problematic, the family coping mechanisms have a protective effect on relationship satisfaction (Didericksen et al., 2015). Mothers who give birth preterm are under more psychological stress than other mothers are. A study by Bener (2013) on 1,659 mothers found that the rate of postpartum depression was 17.3% among the mothers of term infants, while it was 29.4% among the mothers of preterm infants.
Anxiety is a complex confluence of unpleasant emotions and cognitions that are similar to fear but are vaguer and associated with a sense of apprehension (Barlow, 1988). In their study, Zelkowitz et al. (2007) reported that 50% of mothers whose preterm infants had been admitted to the NICU showed symptoms of severe anxiety and depression. Anxiety is more common among mothers who give birth to preterm babies because of their concerns for the future; for instance, such mothers tend to be concerned about whether the baby will survive or have any permanent health problems in a way that mothers of term infants are not. Bener (2013) reported that the rates of anxiety and depression among the mothers of term and preterm infants were 11.6% and 26.5%, respectively (Bener, 2013).
Pace et al. (2016) carried out a study to compare the parents of 150 infants born at under 30 gestational weeks and 151 term infants born after 37 weeks. They reported that 50% of parents of preterm infants showed severe anxiety symptoms shortly after birth. Although a decrease in anxiety symptoms was observed around 12 weeks, it was noted that the rate did not fall below 22% for mothers or 25% for fathers. Even 6 months after birth, parents of preterm infants were at higher risk of depression and anxiety compared with parents of term infants. Although it was not one of the goals of the study to compare the levels of depression and anxiety of mothers and fathers, the symptoms were found to be similar in both parents. This result was surprising because previous studies had shown that fathers had lower levels of distress (Pace et al., 2016).
Trauma is defined as distressing or disturbing events experienced by individuals or their loved ones that hurt or damage their physical and mental wellbeing in various ways (Ozturk & Ulusahin, 2016). Although an individual may not experience it firsthand, witnessing such a damaging event can also be traumatic. Traumatic events are of a dangerous or damaging nature; they occur suddenly and lead to fear, anxiety, withdrawal, and avoidance (Turksoy, 2003). When experiencing trauma or an unwanted change, individuals can present three types of psychological reactions, which are as follows: post-traumatic stress disorder (PTSD), resilience/recovery, and post-traumatic growth (PTG; Hefferon & Boniwell, 2011).
Trauma’s impact on mental health is not always negative. In his book titled Man’s Search for Meaning, Viktor E. Frankl (1946/2006) – the founder of logotherapy – stated that people can change their attitude towards their faith if they find meaning in their suffering. According to Frankl, people begin changing to convert a personal tragedy into growth only when the situation becomes inevitable. Individuals can experience a positive transformation following a traumatic experience. PTG is described as improvements that occur after highly stressful life crises (Calhoun & Tedeschi, 1999). It usually manifests in changed priorities in life, perceiving life to be more valuable, realizing one’s own power, establishing more intimate relationships, gaining awareness of personal strength, and developing a better understanding of spiritual matters. Hospitalization of an infant in neonatal intensive care involving the risk of death is a traumatic experience for that infant’s parents (Affleck & Tennen, 1991). A considerable portion of these parents experience acute stress disorder and/or PTSD (Barr, 2010). However, some parents report surviving the challenge of having an infant in the NICU and emerging from the experience even stronger. Büchi et al. (2007) studied PTG and grief among parents who have lost their premature baby, and mothers were found to experience more intense grief and PTG than fathers did. It was also found that the psychological resilience of the mothers who had children in the NICU related to their growth in this process, and various suggestions were presented to increase this growth (Lee & Kang, 2020).
Bringing the baby into the family system affects the family atmosphere and the couple’s relationship dynamics. If one or both parents perceive the baby as an emotionally and behaviorally difficult baby who is difficult to calm down, the stress of parenting increases. This has a negative impact on the parents’ relationship quality (Berryhill et al., 2015).
Researchers suggest that babies growing up in families involving incompatible and angry marital interactions will have difficulty organizing their emotions in stressful situations (Berryhill et al., 2015). Continuous highly emotional stimulation leads to a disorganized relationship between the baby and parents and an inability to self-regulate emotionally on the child’s part. A study involving 38 married couples and their 3-month-old babies revealed that the parents, who should be a natural source of relaxation for babies, may paradoxically become triggers of negative emotions, such as fear and anxiety. It is clear that the quality of the relationship between parents is important in terms of ensuring babies’ emotional regulation (Owen & Cox, 1997).
Considering the physical, emotional, social, and financial challenges associated with preterm birth, having a marital relationship with strong dynamics is clearly important for the health of the parents and the attention and care they provide to their baby during the NICU stay. It is important for parents to maintain their wellbeing as individuals and as a couple by preserving their relationship satisfaction and emotional connection despite the challenges they face as parents after their baby is discharged from hospital. In this way, parents can provide adequate care to meet premature babies’ needs, which are far greater than term babies’ needs and include therapies, treatments, and developing a secure attachment in this sensitive period of development.
The aim of this study is to examine the depression, anxiety, stress, and PTG experienced by parents after preterm birth from the perspective of relationship dynamics. To achieve this purpose, the study examines whether depression/anxiety/stress has a mediating role between relationship dynamics and PTG, seeking to answer the following research questions:
Do depression, anxiety, and stress after preterm birth play a mediating role between the relationship satisfaction of parents of preterm babies and their PTG levels?
Do depression, anxiety, and stress after preterm birth play a mediating role between the emotional dependency of parents of preterm babies and their PTG levels?
PARTICIPANTS AND PROCEDURE
PARTICIPANTS
The initial number of participants in the study was 1,828 (Figure 1). Data were collected online using Survey Monkey forms. The inclusion criteria were as follows: being a married mother or father of a preterm infant born at or before 32 gestational weeks, a singleton birth, a baby of not more than 12 months old, and a lack of congenital anomaly in the baby. Our rationale for including the parents of infants born at or before 32 weeks is that they make up the group with the highest risk of long-term health problems (Keller et al., 2011). In addition, in many low-income countries, only 30% of neonates born at this stage survive, with almost all infants < 28 weeks dying in the first days of their lives (Blencowe et al., 2012). As illustrated in statistics published by the Turkish Ministry of Health, in 2017, 56.2% of infants born at < 32 weeks did not survive (Turkish Ministry of Health, 2017). We think that the parents of the most vulnerable babies are at greater risk due to the mortality and morbidity rates.
The parents who participated in this study were not necessarily couples. They should not have been diagnosed with any mental disorders because the study includes depression, anxiety, and stress as mediating variables between PTG and relationship dynamics – namely, relationship satisfaction and emotional dependency. We think that any mental health disorder may be a confounding factor when responding to the relevant scales. For this study, 209 individuals with preterm babies, including 159 women (76.1%) and 50 men (23.9%), were included in the analyses based on the inclusion criteria. The age ranges of the participants were 20-40 years for women and 24-50 years for men, with a mean age of 31.01 years (SD = 5.35). Of the participants, 121 (57.9%) were employed, whereas 88 (42.1%) were not. Twenty-one participants (10%) described their income level as inadequate, 95 (45.5%) as partially adequate, and 93 (44.5%) as adequate. When asked whether they or their spouses had had a miscarriage, 46 participants (22%) responded yes, and 163 (78%) responded no. The age distribution of infants in the study was as follows: < 1 month, n = 34 (16.27%); 1-3 months, n = 39 (18.66%); 4-6 months, n = 48 (22.97%); 7-9 months, n = 51 (24.40%); and 10-12 months, n = 37 (17.70%). The age distribution was unimodal and slightly skewed to the left.
DATA COLLECTION TOOLS
Sociodemographic form. The sociodemographic form was developed by the researchers to collect information about the parents of preterm infants. The form included questions about the gender and age of the participants; duration of their marriages; employment status of participants and their spouses; level of income; whether major grief had been experienced in the last year outside the preterm birth, such as in the case of job loss, severe disease, accident, or death of a loved one; whether the participants or their spouse had had a miscarriage; whether they had previously lost a baby; the chronological age of the baby at the time of completing the form; the week of birth of babies; whether babies had any congenital anomalies; whether the participants had another child; whether the participants or spouses had previously given birth to a preterm baby; whether the participants or spouses experienced the threat of preterm birth during pregnancy; whether participants had been diagnosed with a mental disorder; and whether participants considered preterm birth as a traumatic event.
The Relationship Assessment Scale. The Relationship Assessment Scale (RAS) was developed by Hendrick et al. (1998) to measure satisfaction in romantic relationships. The scale was adapted into Turkish by Curun (2001). The seven-item assessment uses a 7-point Likert scale. Factor analysis has revealed one general factor, and the internal consistency coefficient of the scale is .86. A high score on the scale suggests a high relationship satisfaction. The Cronbach’s α internal consistency coefficient of the scale was found to be .90 for this study.
The Emotional Dependency Scale. The Emotional Dependency Scale was developed by Buunk (1981) and adapted to Turkish culture by Karakurt (2001). It measures comparison levels for alternatives, as well as degrees of attachment and interdependency (Buunk, 1995). The nine-item instrument is scored on a 7-point scale. The Cronbach’s α value of the original scale was .81. The Turkish version of the scale has one factor, with a variant of 48.2%. The Cronbach’s α internal consistency coefficient of the scale was found to be .92 for this study.
Post-Traumatic Growth Inventory. The PTG Inventory was developed by Tedeschi and Calhoun (1996) to evaluate the changes people experience after a traumatic experience, and it is made up of five factors and 21 items. A high score on the scale suggests that the individual experiences a high level of growth in the relevant factor. The inventory was adapted into Turkish by Duru (2006). The Cronbach’s α internal consistency coefficient of the Turkish adaptation of the inventory was .93, and the total variant of the five-factor structure was 67.84%. The Cronbach’s α internal consistency coefficient of the scale was found to be .92 for this study.
The Depression, Anxiety, and Stress Scale. The Depression, Anxiety, and Stress Scale distinguishes anxiety, depression, and stress in terms of the dimension and category. This scale, which was developed by Lovibond and Lovibond (1995) and adapted to Turkish by Bilgel and Bayram (2010), is made up of 42 items and uses a 4-point Likert scale. For the internal consistency of the scale, the Cronbach’s α coefficients were calculated as .92, .86, and .88 for depression, anxiety, and stress, respectively. In terms of validity, the root mean square error of approximation (RMSEA) was calculated as .08, goodness of fit index (GFI) as .79, and comparative fit index (CFI) as .75 based on confirmatory factor analysis. The Cronbach’s α values for the internal consistency coefficients of the scale were found to be .86, .89, and .90 for the factors of depression, anxiety, and stress, respectively, for our study.
DATA COLLECTION AND ANALYSIS
The study procedures were approved by the Research Ethics Board of Uskudar University, no. 61351342/2019-313 dated 31.05.2019. The data were collected between March 2019 and February 2020, before the COVID-19 pandemic.
The study design is correlational and aims to determine the presence and/or degree of change between two or more variables (Karasar, 2012). Structural equation model analysis was used to analyze the data. Before evaluating the intervention models, the correlations between the variables were analyzed using the Pearson correlation coefficient. Then, the mediation models were tested in line with the research questions. These models were analyzed using the regression-based bootstrapping technique via the PROCESS macro developed by Hayes (2018). With general use, models were developed to perform 5,000 bootstraps, and bootstrapping coefficients and confidence intervals were created. To ensure the significance of results, the upper and lower limits of the confidence intervals were analyzed, and it was concluded that the analysis was significant when these limits did not cover zero (Preacher & Hayes, 2008).
RESULTS
FINDINGS ON DIFFERENCES BETWEEN MOTHERS AND FATHERS BY VARIABLE
An independent-sample t-test was performed to determine whether the variables involved in the study differed significantly by gender. Related findings are presented in Table 1.
Table 1
Variables in mothers and fathers
Table 1 shows the mean values and SDs based on the scores of the participating mothers and fathers. According to the findings, relationship satisfaction (t = 0.66, p = .512), emotional dependency (t = 1.69, p = .093), and stress (t = 1.80, p = .073) scores of mothers and fathers did not differ significantly. In contrast, there were significant differences in PTG (t = 2.31, p = .022), depression (t = 2.99, p = .003), and anxiety (t = 2.79, p = .006). This shows that the levels of PTG, depression, and anxiety of mothers were higher than those of fathers.
RESULTS OF CORRELATIONS BETWEEN VARIABLES
In the study, which examined depression, anxiety, stress, and PTG experienced by parents with a preterm infant from the perspective of relationship dynamics, the first step was to analyze the correlations among variables. The Pearson correlation coefficients are presented in Table 2.
Table 2
Correlations with variables
As shown in Table 2, the relationship satisfaction and emotional dependency (r = .69, p < .001) experienced by parents following the birth of a preterm baby had a positive correlation with PTG (r = .20, p = .005). In contrast, a negative correlation was found between relationship satisfaction and depression (r = –.45, p < .001), anxiety (r = –.25, p < .001), and stress (r = –.27, p < .001).
A significant positive correlation was found between the emotional dependency and PTG of parents after having a preterm infant (r = .29, p < .001). In contrast, a significant negative correlation was found between emotional dependency and depression (r = –.33, p < .001) and stress (r = –.16, p = .021) of parents. Finally, no significant correlation was found between emotional dependency and anxiety (r = –.10, p = .164). Whereas PTG experienced by parents with preterm infants after preterm birth had a negative significant correlation with depression (r = –.17, p = .017), it did not have a significant correlation with anxiety (r = –.04, p = .579) or stress (r = –.08, p = .243).
FINDINGS FROM THE MODEL TESTING
Regression-based bootstrapping analysis was performed to determine whether depression, anxiety, and stress experienced by parents with preterm infants after preterm birth mediated relationship satisfaction and PTG levels. Figure 2 shows the findings of the model developed to test the mediation of depression, anxiety, and stress in the connection between relationship satisfaction and PTG.
Figure 2
Mediation of post-preterm birth depression, anxiety, and stress between the relationship satisfaction and post-traumatic growth of parents of preterm infants
Note. **p < .001, non-standardized coefficients
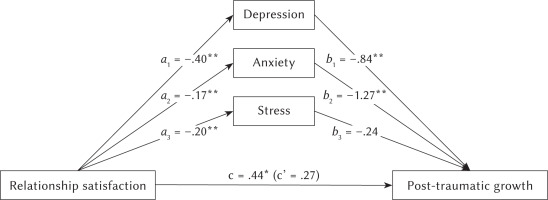
Figure 2 primarily shows direct effects. The relationship satisfaction of parents of preterm infants directly, negatively, and significantly predicts depression following preterm birth (B = –.40, p < .001). Similarly, relationship satisfaction directly, negatively, and significantly predicts both anxiety (B = –.17, p < .001) and stress (B = –.20, p < .001) following preterm birth. In addition, it was found that depression (B = –.84, p < .001) and anxiety (B = –1.27, p < .001) following a preterm birth directly and negatively predict PTG, while stress (B = –.24, p = .280) does not directly predict PTG.
The total effect of the relationship satisfaction of parents of preterm infants on PTG was found to be .44 and significant. However, with the addition of the mediating variables of depression, anxiety, and stress into the model, this effect dropped to .27, which is insignificant. In this respect, there was full mediation. The bootstrapping coefficient and 95% confidence intervals (CIs) of the mediation and significance of the effects of the model shown in Figure 2 are presented in Table 3.
Table 3
Bootstrapping results for the mediation of depression, anxiety and stress between relationship satisfaction and post-traumatic growth
| Indirect effect | Bootstrap coeficient | SE | 95% CI | R2 | (4, 204) | |
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| RS → Depression → PTG | .35 | .14 | .11 | .64 | .10 | 5.65** |
| RS → Anxiety → PTG | –.22 | .07 | –.38 | –.08 | ||
| RS → Stress → PTG | .05 | .07 | –.09 | .19 | ||
As revealed by Table 3, the model developed for PTG was found to be significant [F(4, 204) = 5.65, p < .001]. Mediators in the models showed that post-preterm birth depression has a full mediating role between the relationship satisfaction of the parents of preterm infants and PTG (bootstrap coefficient = .35, 95% CI [.11, .64]). Similarly, it was found that post-preterm birth anxiety has a full mediating role between the relationship satisfaction of the parents of preterm infants and PTG (bootstrap coefficient = –.22, 95% CI [–.38, –.08]). In contrast, it was found that post-preterm birth stress does not have a significant mediating role between the relationship satisfaction of the parents of preterm infants and PTG (bootstrap coefficient = .05, 95% CI [–.09, .19]).
Regression-based bootstrapping analysis was performed to determine whether depression, anxiety, and stress experienced by parents with preterm infants after preterm birth mediated emotional dependency and PTG levels. Figure 3 shows the findings of the model developed to test the mediation of depression, anxiety, and stress in the connection between emotional dependency and PTG.
Figure 3
Mediation of post-preterm birth depression, anxiety, and stress between the emotional dependency and post-traumatic growth of parents of preterm infants
Note. *p < .05, **p < .001, non-standardized coefficients
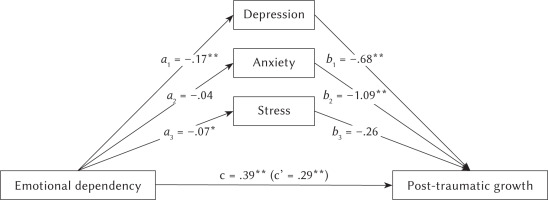
Figure 3 primarily shows direct effects. Emotional dependency of parents of preterm infants directly, negatively, and significantly predicts depression following preterm birth (B = –.17, p < .001). Similarly, emotional dependency also directly, negatively, and significantly predicts stress (B = –.07, p = .044) following preterm birth. In contrast, emotional dependency does not significantly predict anxiety (B = –.04, p = .445).
The total effect of the emotional dependency of preterm infants’ parents on PTG was found to be .39 and significant. However, with the addition of the mediating variables of depression, anxiety, and stress into the model, this effect dropped to .29, which is also significant. In this respect, partial mediation was observed. The bootstrapping coefficient and 95% confidence intervals of the mediation and significance of the effects of the model shown in Figure 3 are presented in Table 4.
Table 4
Bootstrapping results for the mediation of depression, anxiety, and stress between emotional attachment and post-traumatic growth
| Indirect effect | Bootstrap coeffcienti | SE | 95% CI | (4, 204) | ||
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| ED → Depression → PTG | .12 | .06 | .02 | .24 | .12 | 7.57** |
| ED → Anxiety → PTG | –.04 | .03 | –.10 | .02 | ||
| ED → Stress → PTG | .02 | .03 | –.03 | .08 | ||
As revealed by Table 4, the model developed for PTG was found to be significant [F(4, 204) = 7.52, p < .001]. Mediators in the models showed that post-preterm birth depression has a partial mediating role between the emotional dependency of preterm infants and PTG (bootstrap coefficient = .12, 95% CI [.02, .24]). In contrast, it was found that post-preterm birth anxiety (bootstrap coefficient = –.04, 95% CI [–.10, .02]) and stress (bootstrap coefficient = .02, 95% CI [–.03, .08]) do not have a significant mediating role between the emotional dependency of preterm infants and PTG.
DISCUSSION
The relationship dynamics of parents are considered decisive and important factors in dealing with the news of preterm birth, labor, lifelong health risks faced by the infant in the NICU, and the challenges brought about by discharge and care at home (Behrman & Butler, 2007; Hodek et al., 2011). Indeed, it is clear that the strength and accessibility of the couple’s resources in the relationship are as crucial as their individual resources in determining how challenging the process will be. This study shows that the dynamics of the relationship between parents also affects whether they can overcome the approaching physical, mental, financial, and social challenges associated with having a preterm infant.
RELATIONSHIP SATISFACTION AND POST-TRAUMATIC GROWTH
The evaluation of the study findings revealed that based on the direct effects, relationship satisfaction of parents following preterm birth can directly predict depression, anxiety, and stress in a negative and significant way. This finding is consistent with research conducted outside of Turkey (Beach et al., 1990; Ionio et al., 2016; Sokolski & Hendrick, 1999). In Ozturk and Aydin’s (2017) study, marital problems are listed among the psychosocial risk factors affecting perinatal depression. Similarly, in the studies by Sokolski and Hendrick (1999) and Beach et al. (1990), it was found that the risk of depression increases when spouses, regarded as the most important resource in terms of social support, are unable to provide each other with the needed support in marriages that are defined as low quality.
In their study of 160 married couples, Sokolski and Hendrick (1999) reported that intrapersonal factors, such as commitment and love; interpersonal factors, such as self-disclosure; and environmental factors, such as stress affect marital satisfaction. A study conducted in Italy (Ionio et al., 2016) showed that fathers assume the roles of understanding and calming mothers and regulating life outside the NICU; in this context, mothers are faced with stressors related to frequent NICU visits, whereas fathers are unable to attend as frequently because of restricted visiting.
In terms of relationship dynamics, it has been revealed that communication skills and mutual support of partners are among the strongest factors (Hazan & Shaver, 1987; Litzinger & Gordon, 2005; Sokolski & Hendrick, 1999). A study examining the factors affecting the bereavement and PTG of women who had miscarriages found that supportive communication by the spouse and emotional disclosure are among the most important factors predicting PTG (Tian & Solomon, 2018). Caring about spouses’ emotions, encouraging them to express these emotions clearly, listening to their thoughts and emotions without being critical, approving of their feelings, and making eye contact are considered supportive communication practices by a spouse. These supportive engagements allow individuals to make sense of their loss, express it by reframing, and feel worthy again.
In terms of indirect variables, the effect of relationship satisfaction on PTG was found to be .44. With the addition of the mediating variables of depression, anxiety, and stress, this effect dropped to .27, which is insignificant. The findings indicate that this variable has a full mediating role. It is thought that among preterm infant parents, the full mediating role depression and anxiety play is caused by subjective perceptions of parents, such as the baby’s risk of dying and high levels of anxiety about the future and other factors, such as additional diagnoses the baby might have apart from being preterm.
In their study, Schless et al. (1974) found that depressed people perceive themselves to be more vulnerable to family-related problems and view their experiences as more threatening than they really are; moreover, their capacity to adapt to changes is much lower than that among people without depression. It is thought that having a complicated and high-risk pregnancy before preterm birth and how traumatic the birth is perceived to have been affect the development of depression and anxiety along with the intensity of these disorders. These parameters define the full mediating role of depression and anxiety between relationship satisfaction and PTG. This finding reveals that no matter how high the relationship satisfaction of the parents, a mother or father being depressed or having high anxiety prevents PTG.
Although depression and anxiety mediate fully between the parents’ relationship satisfaction and PTG, the study found that stress does not play a significant mediating role in this context. This finding contradicts several studies (Lazarus & Folkman, 1984) that have shown how stress affects individuals’ adaptation skills, such as problem solving and somatic health. In his article, Viner (1999) reviewed the literature related to stress, beginning with Selye, and he described stress as a physiological response to stressors that can be mitigated via individuals’ coping mechanisms. Numerous studies have defined depression as a psychopathological state and a potentially life-threatening affective disorder (American Psychiatric Association, 2013; Bondy, 2002). Anxiety is also described in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) of the American Psychiatric Association (2013) as a disorder where individuals find it difficult to control their worry. The high stressor effects of certain experiences noted in Lazarus and Cohen’s (1977) study, such as giving birth or the danger of a loved one dying, were not verified from the perspective of the mediation of stress on relationship satisfaction and PTG considered in the present study. A possible explanation of this result is that stress is a challenge that is relatively easy to cope with compared with anxiety and depression.
EMOTIONAL DEPENDENCY AND POST-TRAUMATIC GROWTH
According to the findings of our study related to emotional dependency and PTG, when direct effects are considered, emotional dependency of the preterm infants’ parents negatively and significantly predicts postpartum depression. Similarly, emotional dependency negatively and significantly predicts stress but does not significantly predict anxiety.
When evaluating the direct effects, the main factors of emotional dependency are considered, and it is thought that the positive emotions shared by the parents about their premature babies, such as love, bonding, and affection; shared negative emotions, such as fear, concern, and despair; and the parents seeing each other as the most significant source of support and becoming attachment figures for each other may be the main factors that support the results of this study (Feeney, 2007). In their study, Ozturk and Aydin (2017) found that one of the key psychosocial factors linked to perinatal depression is having marital problems. This suggests that a strong feeling of love, dependency, and intimacy between spouses will reduce such marital problems.
In their study, Schless et al. (1974) reported that individuals who suffered from depression were much more vulnerable to marriage- and family-related stressors. Our findings suggest that parents with high levels of emotional dependency may be less exposed to marital stressors; we predict that this can reduce the risk of depression.
Relationship satisfaction and emotional dependency, which were found to positively predict PTG in parents of preterm infants following preterm birth, are auxiliary factors in helping parents to make a positive and sensible assessment of how grave the situation is after they face the new reality they experience following the trauma of preterm birth. According to Frankl (2006), to turn a personal tragedy into victory, people must change when they face a situation that cannot be changed. In line with the study findings, parents with high levels of emotional dependency can change their view and see things from a more positive perspective. The concept of optimism, which focuses on the outcomes of a traumatic event and the positive outcomes that will emerge with it, is part of PTG; this suggests that parents with harmonious relationships and emotional dependency can be successful in guiding each other’s subjective perceptions to a positive and hopeful path.
The literature on emotional dependency and anxiety-related studies reports that many parents of preterm infants suffer from high levels of anxiety (Bener, 2013; Pace et al., 2016; Zelkowitz et al., 2007). In contrast, Kemer et al. (2016) noted that emotional dependency is a positive and strong predictor of relationship satisfaction. Although the results of our study on relationship satisfaction showed that this satisfaction is a negative predictor of anxiety, the results we obtained for emotional dependency contradict this view. Even if emotional dependency is high, it cannot negatively predict anxiety experienced by parents of a preterm infant.
When we observed the indirect effects, it was found that the addition of depression, anxiety, and stress to the model as mediating variables reduced the total effect to .29, which is significant. In this respect, partial mediation was observed. In this study, post-preterm birth depression had a partial mediating role between the emotional dependency of preterm infants’ parents and PTG, whereas the mediating effect of stress and anxiety was not significant. A meta-analysis showed that the frequency of depression among mothers of preterm infants, especially in the first year after birth, was significantly higher than that in mothers of term infants (Vigod et al., 2010).
In their study, Alexopoulou et al. (2018) reported that depression is triggered when parents disregard their emotional needs and focus only on their baby if the baby has a life-threatening condition or is in poor health. In line with this study’s findings, parents who neglect their own emotional needs are unable to achieve the transformation and change in functionality defined by Tedeshi and Calhoun (2004) as PTG.
The indirect effects show that post-preterm birth anxiety and stress do not have a significant mediating role between the emotional dependency of the parents of preterm infants and PTG. That high emotional dependency can be achieved by accepting and responding to the spouse’s attachment needs, as noted in the literature, is in line with this study’s findings (Feeney, 2007).
Possible adverse effects of anxiety and stress on PTG can be overcome in parents with high emotional dependency via more effective communication between the parents and better adaptation to each other, as shown by Cirhinlioglu et al. (2017). The partial mediating role of depression between emotional dependency and PTG shows that dependency between couples is a more significant variable in PTG than relationship satisfaction is.
In their study, Lasiuk et al. (2013) noted three factors that affect the ability of parents of preterm infants to adapt to the new reality, which are as follows: the couple’s individual and collective resources, the quality of the relationship with the NICU team, and the availability of social and functional support. According to Bowen (1978), all members of a family are interconnected, and each member of the system affects the others. Therefore, relationship dynamics are as detrimental as the individual resources of the spouses in how parents will experience the period following preterm birth. Couples with a functioning family structure will understand each other socially and emotionally, interact with interest and love, and keep moving forward no matter what hardship comes their way.
Throughout their relationship, all couples create common resources in various areas that they and the other party can benefit from. It is easy and fast to access these resources. Our study revealed that the relationship resources of parents of preterm infants, and especially their emotional dependency, help them overcome the stressful birth and postpartum periods and are highly effective in turning the crisis period into a positive development. It is understood that emotional dependency and relationship satisfaction have protective effects on depression, anxiety, and stress, in addition to positively predicting PTG.
CONCLUSION, LIMITATIONS, AND FUTURE DIRECTIONS
The purpose of this study was to examine the impact of the relationship dynamics of parents with preterm infants on post-preterm birth depression, anxiety, stress, and PTG. The study showed that post-preterm birth depression and anxiety experienced by parents of preterm infants had a full mediating effect between their relationship satisfaction and PTG levels. The study also demonstrated that postpartum depression experienced by parents of preterm infants played a partial mediating role between their emotional dependency and PTG levels.
There are some limitations of this study that need to be acknowledged. First, our study covered accessible parents with preterm infants in Turkey, and the number of fathers reached was quite low compared with the number of mothers. This situation can be considered the most important limitation of the study. It is recommended that the findings of the study be tested in a larger sample, with more fathers participating, and in different cultures. Another limitation is that the educational status of mothers and fathers was not considered as a variable in the study. In subsequent studies, the educational status of the parents can also be considered as a variable. Here, the stress, anxiety, and depression levels of the parents were considered as variables. That the traumatic effects of having a premature baby were not addressed can be seen as a limitation: This study focused on PTG, but subsequent research may focus primarily on measures of parental trauma levels. In addition, the results of the study can be retested according to the infants’ characteristics, such as the gestational birth week, future risk factors, and post-discharge developmental and health problems. Long-form and self-administered questionnaires are frequently left unfinished (Andreais & Kartsounidou, 2020), and we observed this phenomenon in our survey. Those who did not complete the survey might have significant value for our study. Finally, conducting an online survey carries the risk of selection bias (Blumenberg & Barros, 2018), and this might affect the representation of participants who live in rural areas and/or have limited internet access.
In addition to today’s medical understanding of how to keep preterm infants alive and discharge them without any sequelae, it is clear that family members also need one another in the sense of psychological support. The study findings revealed the importance of establishing family- and baby-centered neurodevelopmental NICUs. Both parents being present can reduce the strain on their relationship dynamics and allow mothers and fathers to serve as primary caregivers rather than merely visitors; as a result, a two-way bond can form between the parents and the baby.
It is thought that having healthcare professionals, primarily nurses and doctors, make observations about the relationship dynamics of parents during their stay at the NICU and guide them to receive psychological support if they perceive weaknesses in the relationship – since this predicts possible risks with regard to depression, anxiety, and stress – will uphold the functionality of families. The nature of the family dynamic an infant will experience after discharge is pivotal in its effect on the ongoing therapy, treatment, and possible developmental problems that could emerge in the future.
It is important to develop and give early intervention and psychological first aid training to parents before discharge of the infant; this should focus on the biopsychosocial development of preterm infants, who may need responsive parenting and timely, adequate, and constant attention much more than term infants do. Following discharge, in addition to routine checks of infants, it is also important to measure the variables and stress factors of couples’ dynamics and guide those with high risk toward psychiatric outpatient services and/or psychotherapy. In future studies, it would be helpful to analyze the effects of the relationship dynamics of parents on the critical developmental processes of preterm infants. In addition, it would be beneficial for the literature and experts working in the field to investigate how the relationship dynamics of preterm infants’ parents change in the coming years.



