BACKGROUND
Rheumatoid arthritis (RA) is recognized as one of the most common and severe joint diseases (Briggs et al., 2013). It is characterized by chronic and progressive joint inflammation, often leading to severe pain (Coty & Wallston, 2010; van der Woude & van der Helm-van Mil, 2018). Not only is RA incurable, but it can also rapidly progress and impair agility, mobility, and physical function, potentially resulting in disability (Martinec et al., 2019; van der Woude & van der Helm-van Mil, 2018). As a result, the disease negatively impacts the patient’s quality of life and emotional well-being (Bouhouche et al., 2017; Druce et al., 2018; Hashimoto et al., 2020; Kostova et al., 2014; Rice et al., 2016). Among the various symptoms of RA, patients commonly identify pain as the most prominent and severe (Englbrecht et al., 2012). Prolonged inflammation often leads to chronic pain, significantly disrupting daily activities and overall lifestyle (Anderson, 2001). Patients struggle to engage in physical activities, perform daily tasks, and maintain a normal routine. Consequently, pain causes substantial stress and further compromises the patient’s quality of life and emotional well-being (Bouhouche et al., 2017; Kostova et al., 2014; Rice et al., 2016).
Empirical data highlight that chronic pain, including that associated with RA, poses a significant global health challenge (Martinez-Calderon et al., 2018). Despite this, the scientific literature reveals that many questions regarding pain manifestation and control remain unanswered (Martinez-Calderon et al., 2018). Specifically, there is a lack of knowledge concerning psychosocial factors associated with pain severity (Rolbiecki et al., 2017). When studying the challenges faced by patients with RA, researchers focus on the variations in disease progression. While RA presents difficulties and obstacles for most patients, individuals respond to them differently. Some patients resist accepting life changes and strive to reclaim their former life, making little effort to manage the disease and pain. In contrast, others quickly adapt to their altered health condition and adjust to new circumstances. They proactively modify their lifestyles, exerting considerable effort to minimize disease manifestation and pain while pursuing personal goals despite the pain (Akbari et al., 2016; Kostova et al., 2014). Consequently, researchers inquire about the factors contributing to such differences among patients and the phenomena associated with better adjustment and less severe pain. Several studies suggest that various psychosocial factors may influence pain manifestation among patients with RA (Bergström et al., 2023; Bouhouche et al., 2017; Rezaei et al., 2014; Vendrusculo-Fangel et al., 2022).
Empirical data demonstrate that high self-efficacy can assist individuals in adapting to changing circumstances and overcoming challenges, including pain (Martinez-Calderon et al., 2020; Moyano et al., 2019). As a result, many researchers highlight pain self-efficacy (PSE) as a potential factor associated with decreased pain intensity (van der Maas et al., 2012; Nash et al., 2013; Rolbiecki et al., 2017; Sturgeon & Zautra, 2010). Some studies suggest that individuals who have greater trust in their ability to manage pain tend to experience less intense pain, regardless of the underlying cause (Gligorov, 2018). Conversely, others link PSE to better adjustment to pain, making it easier to endure, without necessarily reducing the pain intensity (Ahmed et al., 2019; Rolbiecki et al., 2017). Consequently, the exact impact of PSE on pain manifestation remains somewhat unclear, emphasizing the need for further research exploring the connection between these phenomena (Martinez-Calderon et al., 2020). Additionally, there is empirical evidence indicating that that certain factors, such as disease duration, can influence the association between PSE and pain. For instance, Hashimoto et al. (2020) found that long disease duration was a risk factor for poor quality of life in patients with RA, irrespective of their level of PSE. Galloway et al. (2020) examined data from the Burden of RA across Europe and discovered that the prevalence of pain, activity impairment, and work limitations increases with the severity of RA, particularly in patients with long-standing RA. These findings highlight the importance of considering disease duration as a potential moderator when investigating different variables among RA patients.
Psychosocial factors, including the emotional support of a partner, can also influence pain experienced by individuals. Research indicates that emotional support assists patients with RA in adapting to the disease (Bergström et al., 2023; Coty & Wallston, 2010), overcoming various disease-related challenges (Fallatah & Edge, 2015), and potentially reducing pain intensity (Coty & Wallston, 2010; Pow et al., 2018). It has been observed that individuals who lack support from their relatives often experience more severe disease symptoms and intense joint pain (Karlsson et al., 2006). However, the relationship between pain and emotional support is complex. According to Lopez-Martinez et al. (2008), while individuals with chronic pain who receive more support tend to experience less stress, better pain control and reduced pain intensity, certain types of support can exacerbate the pain experienced by patients. Constant support and attention from a spouse, for example, can be perceived as overwhelming or excessive, leading to feelings of hopelessness (Lopez-Martinez et al., 2008). Similarly, other authors argue that the perception and severity of pain may be influenced by the reactions of those around the person in pain (Akbari et al., 2016). Often, individuals witnessing someone in pain show compassion but tend to catastrophize that pain, perceiving it as more severe than the person actually feels. Meanwhile, excessive attention and assistance can cause stress, reduce self-confidence, and hinder pain management efforts (Akbari et al., 2016). Khan et al. (2009) also note that support, at times, can be perceived by the patient as social control, leading to unintended negative effects and potentially worsening health over time. Excessive support and help may foster dependence and reduce the individual’s motivation to address difficulties independently. Therefore, the authors emphasize that partner support is only beneficial when provided appropriately (Khan et al., 2009). Conversely, inadequate or insufficient support from partners can also impact pain experiences. Research suggest that individuals in pain who do not receive proper support from their partners during the day tend to experience more severe pain the following day compared to those who receive adequate support (Pow et al., 2018).
Based on findings that emotional support may not directly reduce pain severity, some researchers propose that its influence operates through other factors, such as self-efficacy. Holtzman et al. (2004) observed that when individuals in pain receive support from loved ones, they are encouraged to believe in their ability to overcome pain-related challenges. Those who receive support are more likely to take action towards pain relief, leading to better pain adjustment and reduced severity. Empirical evidence demonstrates that emotional support from significant others can enhance self-efficacy and reduce negative emotions associated with pain (Kostova et al., 2014). Providing emotional support to individuals in pain can help alleviate pain-related difficulties, boost confidence in managing pain, and motivate proactive efforts to combat it (Liu et al., 2017).
Building on these empirical insights, the aim of the present study was to address two primary research questions. Firstly, does perceived partner’s emotional support have predictive value for pain severity in women, when included in the same prediction model with pain self-efficacy (PSE)? Although data on emotional support and pain severity in the RA group are somewhat ambiguous, a significant correlation between the variables is typically observed. In contrast, the role of self-efficacy in pain severity is well established, suggesting that it is a robust predictor for patients with various chronic pain conditions. Thus, examining the predictive role of emotional support alongside the strong predictor of PSE can provide insights into the value of perceived partner’s emotional support in women with RA. Secondly, does PSE act as a mediator in the relationship between perceived partner’s emotional support and women’s pain severity? Previous studies support the notion that the impact of emotional support on pain severity in patients may be indirect, through its influence on self-efficacy. Additionally, the analysis considers pain medication and disease duration as control variables, with the latter serving as a potential moderator in the association between PSE and pain severity.
PARTICIPANTS AND PROCEDURE
STUDY PROCEDURE
The research project as well as its ethical aspects were approved by the institutional health psychology review board.
The study was carried out online after creating an electronic version of the survey in the spring of 2020. An invitation to participate in the study along with a link to the survey was posted to various Facebook groups associated with RA (e.g. Arthritis, RA, RA. Let’s recover ourselves, etc.). Those Facebook groups were private, requiring special permission from administrators. The main inclusion criteria were age (30-50 years), declared diagnosis (RA), and ongoing partnership. The age group of 30-50 years old was selected based on information provided by the Arthritis Foundation (n/a). According to the foundation, rheumatoid arthritis (RA) typically begins in women between the ages of 30 and 60, while in men it tends to develop after the age of 45. Additionally, the specific age group of 30-50 years old represents a crucial stage in an individual’s life, characterized by multiple responsibilities, career development, and family commitments. Analyzing the relationship between RA pain and psychosocial factors such as pain self-efficacy and partner’s emotional support helps elucidate the complex interactions that influence pain management and overall well-being in this specific age group. It sheds light on the potential mechanisms through which these psychosocial factors can affect disease outcomes, treatment adherence, and quality of life.
The informed consent, containing essential study information such as the researchers’ details, study objectives, participation conditions and withdrawal options, potential risks and benefits, data protection and confidentiality, as well as contact information, was provided on the first page of the survey. At the end of the informed consent, participants were required to indicate their consent or refusal. Those who declined participation were directed to the final page of the survey, while those who consented were directed to the initial page with selection questions regarding age, diagnosis, and partnership status. If respondents did not meet any of the inclusion criteria, they were not permitted to proceed to the main survey. No incentives or rewards were provided for participating in this study.
PARTICIPANTS
A total of 266 individuals accessed the informed consent page. However, 9 individuals declined to participate in the study, 23 individuals did not fall within the specified age group, and 29 individuals did not report having an ongoing partnership during the study period. A total of 205 respondents met the inclusion criteria and completed the survey. However, since only 9 of them were male, it was decided to analyze the data exclusively for females. Therefore, the final sample comprised 196 women, with an average age of 41.54 years (SD = 6.60). Among the women, the majority were married (n = 124, 64%), 47 women (24%) were in a non-marital partnership but living together, and 24 (12%) women had a partner with whom they did not reside.
In terms of disease duration, it ranged from 1 to 30 years, with an average of 9.72 years (SD = 6.03). A higher proportion of respondents (n = 116, 59%) reported using painkillers to manage their RA pain.
RESEARCH INSTRUMENTS
The survey consisted of four parts:
Control variables: the participants were asked about their age, couple relationship status (married/living in partnership/having a partner but living separately), disease duration (since the diagnosis of RA by a rheumatologist), and use of painkillers for controlling RA pain (non-use/use).
RA Pain Scale (RAPS; Anderson, 2001). The scale comprised 24 items that assessed the frequency of various pain symptoms experienced by the participants over the past week. Each statement was rated on a 7-point scale, ranging from 0 (never) to 6 (always). The scale encompassed four subscales, capturing different components of pain: 1) Physiologic component (5 items; Cronbach α = .83); the subscale measured the clinical symptoms of RA (e.g. stiffness of joints, pain during movement). 2) Affective component (4 items; Cronbach α = .75); the subscale assessed the emotional aspects of the pain (e.g. whether the pain causes severe discomfort, annoyance, or anxiety). 3) Sensory-discriminative component (9 items; Cronbach α = .90); the subscale focused on the nature and characteristics of pain sensations (what type of pain a person feels, how long the pain lasts, how often it recurs, etc.). 4) Cognitive component (6 items; Cronbach α = .84); this subscale examined the impact of pain on a person’s daily life (e.g. how much it limits daily activities, person’s activity, engagement) and how pain affects beliefs about pain control. The total score of the RAPS represented the overall pain severity (24 items; Cronbach α = .95). Higher scores on the scale and subscales indicated greater pain severity.
Communication Based Emotional Support Scale (CBESS; Weber & Patterson, 1996). We utilized an original scale consisting of 20 items, rated on a 5-point scale ranging from 1 (almost never true) to 5 (almost always true). One item was excluded from the analysis due to its small and negative item-total correlation. The 19-item scale encompassed two subscales: 1) Emotional support (11 items; Cronbach α = .89). This subscale assessed the emotional support provided by a partner (e.g. “He helps me work through my thoughts and feelings about major life decisions”; “He says and does supportive things for me when I am feeling down”). 2) Emotional disengagement (8 items; Cronbach α = .87). The subscale measured the extent of emotional disengagement and the lack of emotional support from a partner (e.g. “When I tell my partner about a problem that I am having, he does not seem to be paying attention”; “He avoids me when I am depressed”). The items related to emotional disengagement were recoded, so that higher scores indicated less emotional disengagement (i.e., more support) from the partner. The total score of emotional support provided by the partner was obtained by summing the scores of all 19 items (Cronbach α = .92), with higher scores indicating greater emotional support.
Pain Self-Efficacy Questionnaire (PSEQ; Nicholas, 2007). This self-report measure consisted of 10 items assessing an individual’s confidence in their ability to engage in various activities despite experiencing pain (e.g. “I can enjoy things, despite the pain”; “I can still accomplish most of my goals in life, despite the pain”). Each item was rated on a 7-point scale ranging from 0 (not at all confident) to 6 (completely confident). Higher scores on the questionnaire (Cronbach α = .94) indicated a greater level of confidence in managing and coping with pain.
DATA ANALYSIS
The data were analyzed using SPSS Version 23 and AMOS version 23. To assess the normality of scale distributions, asymmetry and excess coefficients were examined. It was considered that the distribution met the conditions of normality when the coefficients fell between –1 and 1. The results of the study indicated that all scales used in the statistical analysis met the normality conditions, allowing for the use of parametric criteria.
Four hierarchical series of multiple regression analyses were conducted to explore the contribution of study variables in predicting the four subscales of RAPS as dependent variables. Each hierarchical multiple regression analysis included two to three blocks of independent variables, which consisted of the subscales of partner’s emotional support, PSE, as well as control variables (age, disease duration, use of pain medication). Cohen’s f2 was calculated to estimate the effect size for each step of the hierarchical multiple regression. Following Cohen’s guidelines (Cohen, 1988), f2 ≥ 0.02, f2 ≥ 0.15, and f2 ≥ 0.35 represent small, medium, and large effect sizes, respectively.
A mediation analysis was performed to examine the role of PSE as a mediator in the relationship between a partner’s emotional support and RA pain severity. The analysis utilized the maximum likelihood method and assessed several goodness-of-fit indices (Hooper et al., 2008), including model χ2, RMSEA, SRMR, TLI, GFI, and CFI. Acceptable values for TLI, GFI, and CFI were considered to be greater than 0.90, while values exceeding 0.95 were considered excellent. For RMSEA and SRMR, values lower than 0.08 were considered acceptable, with values close to 0.05 considered good (Vandenberg & Lance, 2000). Bootstrap resampling was employed to test the significance of the mediation, using 5000 bootstrap samples and 95% confidence intervals. Furthermore, a moderation analysis was conducted to test the hypothesis that disease duration influenced the strength of correlation between PSE and pain severity. The moderation analysis, including simple slopes and slope plotting, was performed using the Hayes PROCESS 3.5.3 plugin in SPSS (Hayes, 2018).
RESULTS
The means, standard deviations, and Pearson correlation coefficients for all study variables are presented in Table 1. The total score of pain severity and its components showed a negative correlation with PSE and a positive correlation with perceived partner’s emotional support. The data indicate that greater pain severity is associated with lower PSE and higher perceived emotional support from a partner (total score). As the partner’s emotional disengagement and emotional support did not significantly correlate with certain components of pain severity, they were not included in the hierarchical multiple regression analyses when the corresponding component of pain severity was treated as the dependent variable.
Table 1
Descriptive statistics and correlations between components of rheumatoid arthritis pain, pain self-efficacy, and perceived partner’s emotional support among women with rheumatoid arthritis (N = 196)
[i] Note. PS – pain severity (total score of RAPS); PC – physiologic component; AC – affective component; SDC – sensory-discriminative component; CC – cognitive component; PSE – pain self-efficacy; PES – partner’s emotional support (total score of CBESS); ES – emo-tional support; ED – emotional disengagement. *p < .05, **p < .01, ***p < .001.
Subsequently, four two- or three-step hierarchical multiple regression analyses were conducted for each subscale of pain severity as the dependent variable. The variance inflation factors (VIF) and tolerance factors for each predictor variable fell within an acceptable range, with VIF values no larger than 2.25 (ranging between 1.05 and 2.25) and tolerance factors no smaller than 0.43 (ranging between 0.43 and 0.97), suggesting no collinearity among the independent variables. The results of the final regression models are presented in Table 2.
Table 2
Descriptive statistics and correlations between components of rheumatoid arthritis pain, pain self-efficacy, and perceived partner’s emotional support among women with rheumatoid arthritis (N = 196)
The findings revealed that all final models of the hierarchical multiple regression analyses were statistically significant. However, there were variations in the significant independent variables predicting the different components of RA pain. The higher scores of the physiologic pain component were predicted by lower PSE and the use of pain medications. The final model accounted for 20% of the variance in the dependent variable, with a moderate effect size (f2 = 0.27). The inclusion of PSE resulted in a greater change in R2 compared to the block of control variables (0.17 vs. 0.05). Similar results were observed for the cognitive component of pain, but with a large effect size (f2 = 0.43). Lower PSE and the use of pain medications predicted higher scores in this component; the change in R2 was primarily explained by PSE (0.25 vs. 0.05). Participants who reported lower PSE and higher emotional support from their partners had higher scores in the affective component of pain (moderate effect size; f2 = 0.19). The block of control variables did not significantly contribute to the change in R2 (.03, p = .054). Lastly, the three blocks of predictors for the sensory-discriminative component of pain explained 26% of its variance, with a large effect size (f2 = 0.39). Lower PSE, less emotional disengagement from a partner, and the use of pain medications were the strongest predictors, with PSE accounting for the largest change in R2 (0.14; the blocks of partner’s emotional support and control variables contributed 0.09 and 0.05 to the change in R2, respectively).
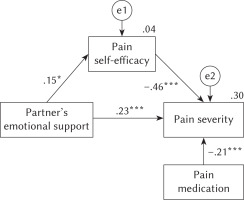
Next, the mediation model was tested. Considering that the variable of pain medication was consistently identified as a strong predictor in all four regression models, we made the decision to control for it by including it in the mediation model. The results of the bootstrap analysis using SEM revealed partial mediation (Figure 1). The model demonstrated a good fit, showing that partner’s emotional support (total score) had both direct and indirect associations with pain severity (total score) through PSE. However, the direct and indirect effects of partner’s emotional support operated in opposite directions. Higher scores of perceived partner’s emotional support predicted higher scores of patient’s PSE, which in turn predicted lower pain severity (higher partner’s emotional support → lower pain severity). Conversely, higher scores of the partner’s emotional support directly predicted greater pain severity (higher partner’s emotional support → greater pain severity).
Figure 1
Path mediation model of relationships between perceived partner’s emotional support, pain self-efficacy, and rheumatoid arthritis pain severity
Note. Standardized regression weights (β), correlations, and R2 are presented. Goodness-of-fit indices: χ2(2) = 3.74, p = .154, CFI = 0.98, TLI = 0.93, GFI = 0.99, SRMR = .046, RMSEA = .067 (90% CI [.00, .17]); *p < .05, ***p < .001
Considering the suggestions from existing literature, the duration of the disease was hypothesized to moderate the relationship between PSE and pain severity. Therefore, a moderation path was added to the mediation model, and a moderated mediation analysis was conducted using the Hayes PROCESS 3.5.3 plugin. The results indicated that the model was statistically significant (F = 18.99, p < .001), and the moderation interaction effect was also significant (p = .045). To aid interpretation, a graph depicting the moderation interactions was plotted, and simple slope analysis was performed. This analysis allowed the evaluation of the impact of the moderator (disease duration) on the relationship between the independent (PSE) and the dependent (pain severity) variable by dividing the data into three levels based on the moderator’s values: low (mean minus 1 standard deviation), moderate (mean) and high (mean plus 1 standard deviation). The levels of the moderator (M = 9.72, SD = 6.02) were categorized as short disease duration (3.70), moderate disease duration (9.72), and long disease duration (15.74). The results of this analysis are presented in Table 3 and Figure 2.
Table 3
Moderation analysis: the effect of disease duration on the association between pain self-efficacy and women’s rheumatoid arthritis pain severity
| Duration of disease | Effect | SE | t | p |
|---|---|---|---|---|
| Short (M – 1 SD) | –1.22 | .18 | –6.83 | < .001 |
| Moderate | –0.95 | .13 | –7.40 | < .001 |
| Long (M + 1 SD) | –0.67 | .19 | –3.59 | < .001 |
Figure 2
The effect of disease duration as a moderator on the association between pain self-efficacy and women’s rheumatoid arthritis pain severity
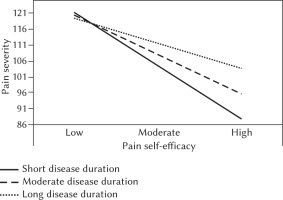
Although the effect of disease duration on the association between perceived partner’s emotional support and women’s RA pain severity was statistically significant in all three levels of the moderator, the simple slope plot (Figure 2) demonstrates that the association varies depending on the level of the moderator. The relationship between PSE and pain severity was strongest in the group with short disease duration, and it weakens as disease duration increases. However, the model remains consistent across all three groups, indicating that lower PSE is associated with higher pain severity.
DISCUSSION
This study aimed to test the assumptions that partner’s emotional support has a significant predictive value for women’s RA pain severity, and that the association between partner’s emotional support and pain severity is indirect, mediated by women’s PSE.
The results revealed that higher PSE was a significant and the strongest predictor of lower pain severity across all RA pain components. However, the predictive value of partner’s emotional support was not as clear, and varied depending on the pain component. Additionally, the use of pain medications significantly predicted three out of four pain components, while disease duration did not have a predictive value for either of the pain components. Lower scores in the physiologic and cognitive pain components were predicted by higher PSE and the use of pain medications. This means that women who feel in control of their RA pain and take pain medications experience less pain during movement, less intense stiffness of joints, and fewer limitations in their daily activities and engagement. These findings align with other empirical data. Mittinty et al. (2018) argue that high self-efficacy is one of the most important factors in reducing the severity of chronic pain. Indeed, many researchers note that higher self-efficacy is associated with less intense pain, better adjustment to pain, and improved pain control (Miles et al., 2011; Ruben et al., 2017; Vendrusculo-Fangel et al., 2022). Sturgeon and Zautra (2010) also observed that high self-efficacy not only reduces the severity of pain in the present moment but also predicts lower pain severity in the future. Recent studies in the context of chronic pain further confirm these results, showing that increasing the self-efficacy in individuals with chronic pain leads to a decrease in pain severity (Ahlstrand et al., 2017; Ahmed et al., 2019). On the other hand, a recently published study by Hashimoto et al. (2020) found that the use of pain medications independently predicts RA patients’ quality of life. The authors suggest that patients’ PSE may be affected by an improved quality of life due to the effect of pain medications on pain severity. However, it is also possible that the use of pain medications reflects a patient’s proactive approach to pain control. An association between PSE and the use of pain medications seems to exist, but further studies are needed to determine the nature of this association, whether it is direct or indirect. In addition to PSE, partner’s emotional support had a significant predictive value for the affective and sensory-discriminative components of pain. However, different elements of partner’s emotional support predicted different pain components. Lower emotional support from a partner and higher PSE predicted lower scores in the affective component of pain. Women who perceive their partners as less helpful and supportive in overcoming various issues and challenges, and who feel more in control of their RA pain, report less severe discomfort, annoyance, and anxiety related pain. On the other hand, women who perceive their partners as more emotionally disengaged (less attentive to their emotional problems), feel more in control of their RA pain, and take pain medications, report less frequent and less persistent pain. These results indicate that a less intrusive and supportive partnership in the context of RA is more beneficial for women in pain. Empirical data on partners’ support outcomes for patients with RA are ambiguous.
Kostova et al. (2014) observed that confidence in a patient’s ability to overcome difficulties can enhance their self-confidence and self-efficacy. It has been noted that individuals who receive support are more likely to take action to relieve pain and make adjustments to reduce its intensity compared to those who do not receive support (Holtzman et al., 2004). On the other hand, Lopez-Martinez et al. (2008) highlight that individuals often direct more support towards their partners when they witness them experiencing chronic pain. Similarly, in their dyadic qualitative research, Bergström et al. (2023) identified a reciprocal dynamic of support between patients with RA and their partners, characterized by a strong sense of mutual availability. However, imbalances occasionally arise between the emotional support received and the support needed within these dyads, indicating that well-meaning significant others can unintentionally cause tension for individuals with RA. Akbari et al. (2016) present similar findings, noting that those providing support often overly emphasize the pain experienced by a patient and sometimes engage in catastrophizing it, perceiving it as more severe than the patient themselves. Consequently, relatives frequently view a person in pain with compassion and tend to provide excessive support, which Khan et al. (2009) even describe as social control. According to them, when the support is excessive, it can have the opposite effect, increasing the dependence of patients on others, reducing their problem-solving abilities and initiative, and undermining their self-confidence. It is plausible that the results of our study precisely reflect this mechanism of the relationship between lower perceived emotional support from a partner and higher PSE in patients with RA. Several factors can explain this observation. Specifically, RA pain is often regarded as one of the most pronounced and severe symptoms of the disease (Englbrecht et al., 2012; Martinec et al., 2019). While the pain caused by rheumatoid arthritis can vary (periodic, localized, or widespread), it typically becomes chronic as the disease progresses (Hashimoto et al., 2020). This means that the pain does not resolve quickly, unlike many other challenging life situations. Consequently, emotional support provided by a partner in prolonged situations may not be as effective as in situations that are resolved quickly or have a relatively short duration. Additionally, an important factor for effective problem-solving (pain control) is the presence of a viable solution. However, empirical data indicate that despite advances in the treatment of inflammatory diseases, pain remains a major issue for RA patients, as there is currently no fully effective treatment to reduce disease activity (Christensen et al., 2016; van der Woude & van der Helm-van Mil, 2018). Therefore, it is likely that a partner’s emotional support may be less effective in such situations compared to situations where quick and effective solutions are available. The negative emotions experienced by women due to pain do not easily subside, as they are aware of the chronic nature of RA and its consequences. Thus, the partner’s emotional support provided by a partner may not effectively assist in coping with the situation. Excessive support can lead to a sense of helplessness, reinforcing a woman’s perception of the complexity of the situation and diminishing her coping abilities.
Mediation analysis revealed that perceived partner’s emotional support has both direct and indirect effects on women’s RA pain intensity, with the indirect effect mediated by PSE. Specifically, higher emotional support from a partner directly increases women’s pain intensity but indirectly increases their PSE, which in turn decreases their pain intensity. While only a few studies have examined similar mediation, these results align with the researchers’ perspective that the partner’s emotional support in the context of patients’ pain may act indirectly. Holtzman et al. (2004) observed that individuals in pain are motivated to believe in their ability to overcome difficulties when they receive support from a loved one. Support from close individuals can enhance patients’ self-efficacy, encouraging them to become more proactive in managing their pain (Liu et al., 2017). Although the direct effects of partner’s emotional support on pain intensity has been discussed before, the most intriguing finding is the opposite direction of the effect when emotional support acts both directly and indirectly. It appears that certain aspects of partner’s emotional support, such as instilling confidence in the patient’s coping abilities, are beneficial for maintaining PSE, while others, such as excessive support and continuous focus on the partner’s pain, can be detrimental. This implies that partners of individuals with RA should be knowledgeable about providing appropriate emotional support. However, our study does not allow us to validate the assumption that partners provide inadequate support, as the emotional support was subjectively assessed by the recipient (women) rather than the provider (partners). Nonetheless, our results align with those obtained by Pow et al. (2018), who conducted dyadic research and observed that partners of patients with RA often provide emotional support inappropriately and exhibit extremes in their support provision (either limited or excessive).
Finally, moderated mediation analysis supported the hypothesis that disease duration can influence the association between PSE and RA pain intensity. We found that as RA duration increases, the association weakens. These findings are in line with some empirical data (Galloway et al., 2020; Hashimoto et al., 2020) demonstrating that long-lasting chronic RA pain may be more resistant to self-efficacy beliefs. On the other hand, there is a possibility that due to enduring pain, patients’ PSE diminishes, as the lack of change in the situation becomes unbearable and leads to frustration and disappointment in their efforts to cope with the pain. Therefore, long-standing chronic RA pain should be considered a risk factor that may reinforce pain itself through indirect mechanisms linking pain with certain buffers, such as PSE.
LIMITATIONS
The study results should be interpreted with caution due to several limitations. First, the inclusion criterion for the study was a diagnosis of RA, and recruitment was conducted through various Facebook groups associated with RA. However, despite efforts to ensure that only respondents with diagnoses confirmed by a rheumatologist could proceed with the survey, online research always carries the possibility of respondents falsifying their data. To mitigate this, it is recommended to conduct similar studies within medical care institutions. By conducting studies in clinical settings, it would be possible to obtain more comprehensive and reliable assessments of individuals with RA. This approach would help ensure accurate diagnosis confirmation and minimize the potential for data falsification. Comparing findings from online surveys with those from clinical settings can provide a more robust understanding of the phenomena under study. Another limitation is that the study was conducted with a sample consisting only of women. Therefore, the results do not provide insights into the male population, where tendencies related to the studied phenomena may differ from those observed in the female population. While statistical data indicate that a significant proportion of men suffer from RA, there is a substantial knowledge gap regarding their experiences, as males are generally less inclined than females to prioritize their health and participate in research. Researchers should strive to overcome the challenges of recruiting men for research and explore their unique perspectives, interactions, and coping strategies. This would contribute to a more comprehensive understanding of RA across different genders and facilitate the development of tailored interventions for male patients. The third limitation pertains to the assessment of partner’s emotional support. In this study, women were asked to report how they perceive the emotional support provided by their partners. While this study design can be valuable for verifying initial assumptions, a dyadic study design is necessary to confirm the tendencies identified in our research. This would involve investigating not only how men support their ill partners but also how their actions contribute to enhancing their partners’ self-efficacy. Additionally, exploring women’s specific responses to their partners’ behaviors and actions can provide valuable insights into the dynamics of emotional support within the context of RA. Furthermore, it is important to acknowledge that the study employed a cross-sectional design, which limits the ability to establish causal relationships. Longitudinal studies would allow for the exploration of temporal relationships and provide a better understanding of how psychosocial factors, such as pain self-efficacy and partner’s emotional support, evolve over time and their impact on pain outcomes and overall well-being in individuals with RA. Finally, due to the lack of medical data, the study was unable to assess the severity of the disease and the degree of disability. To provide a more comprehensive understanding of the impact of RA, future studies should consider incorporating measures of disease severity and disability, such as objective clinical assessments and tools like the Health Assessment Questionnaire (HAQ). This would enable researchers to examine the relationship between these factors and pain experiences, self-efficacy, and support dynamics more accurately.
CONCLUSIONS
Despite its limitations, this study yields significant findings that contribute to our understanding of pain manifestation in women with RA and offer practical insights into providing assistance to those experiencing chronic pain. The study confirms the heterogeneous nature of RA pain, emphasizing the importance of using assessment tools that capture its various components during the treatment process. Given the detrimental impact of chronic pain on individuals’ lives, it remains crucial to emphasize the importance of using assessment tools that capture its various components during the treatment process. The results highlight the significance of both medical treatment and psychological factors, such as PSE and partner’s emotional support, in influencing the manifestation of RA pain. This suggests that interventions aimed at enhancing PSE and providing training for partners should be integrated into the treatment process alongside medical interventions. It is vital for the partners to be able to identify situations where their loved ones require support and assistance, as well as instances where empowering and encouraging them to take action to overcome the challenges of the disease may be sufficient. Consequently, training partners to provide appropriate emotional support, while concurrently strengthening patients’ PSE, can be an integral aspect of rheumatoid arthritis treatment.


