BACKGROUND
The oncology setting is a stressful environment for patients, their families, and healthcare professionals (Jones et al., 2013). Oncology care staff include (but are not limited to): oncologists, radiotherapists, social workers, clinical psychologists, and registered nurses with advanced practice in oncology (oncology nurses). Although each of these groups is at risk of work-related stress (Jones et al., 2013), this review focuses specifically on oncology nurses. The day-today role of oncology nurses varies significantly, from prevention to symptom management, acute care to palliative care, and treatment to rehabilitation (Wyatt & Hulbert-Williams, 2015). Given the diversity of this role, challenging and unpredictable situations occur frequently, often leading to the experience of occupational stress (Jones et al., 2013).
IMPORTANT CONCEPTS IN OCCUPATIONAL WELLBEING
‘Occupational stress’ encapsulates various psychological concepts such as burnout, secondary post-traumatic stress, vicarious traumatisation, and compassion fatigue. Burnout and compassion fatigue are most commonly reported in this population and at high prevalence levels (Domagała & Gaworska-Krzemińska, 2018; Gomez-Urquiza et al., 2016; De la Fuente-Solana et al., 2020). Burnout results from consistent exposure to elevated work-related stress, and is described as consisting of three factors: (i) emotional exhaustion (i.e. a state of being psychologically drained due to exposure to consistent stress), (ii) depersonalisation (i.e. a cynical approach towards the caring role) and (iii) reduced personal accomplishment (i.e. feeling less effective when caring for patients) (Maslach, 1982). Compassion fatigue, or the ‘cost of caring’ (Figley, 1995), refers to the reduction of compassion (i.e. sympathy towards the suffering of others, creating a desire to help) over time, and an increase in hopelessness with regards to carrying out a caring role. This is mainly due to caring for and constantly witnessing patients go through life-limiting illnesses and trauma (Joinson, 1992).
High levels of burnout and compassion fatigue have been reported globally in this population (Cheng et al., 2015; Hooper et al., 2010; Potter et al., 2010; Sherman et al., 2006). Out of 153 oncology nurses in Potter et al.’s study (2010), 37% of inpatient staff reported experiences of compassion fatigue, and 44% reported high levels of burnout. Emotional exhaustion was high in Kutluturkan et al.’s (2016) sample of 140 oncology nurses, and, similarly, in a third of Guveli et al.’s (2015) Turkish sample (n = 159). A study of 216 American hospice nurses reported that around 80% of the sample were at high risk of compassion fatigue (Abendroth & Flannery, 2006). Oncology nurses have reported higher levels of burnout and compassion fatigue compared to other specialties such as emergency, intensive care, and nephrology nurses (Hooper et al., 2010; Ortega-Campos et al., 2020).
WHAT ARE THE CAUSES AND CONSEQUENCES OF BURNOUT AND COMPASSION FATIGUE FOR THIS WORKFORCE?
Barnard and colleagues (2006) list 50 stressors specific to the oncology setting, with a prevalence rate of over 50% within their sample of 101 oncology nurses. Significant positive correlations were found between those stressors and both emotional exhaustion and depersonalisation scores. High workload/caseload (Sherman et al., 2006; Wazqar, 2019), low job autonomy (Escot et al., 2001), emotional demands of patients and their families (Isikhan et al., 2004; Wazqar, 2019), constantly dealing with illness and death (Ekedahl & Wengström, 2007; Florio et al., 1998), and difficult communication with patients (Corner, 2002) all serve to increase oncology nurse stress. These are further exacerbated by the pressures stemming from the current coronavirus pandemic (Abratt, 2020). Recurrent experiences of these stressors further increase risks of burnout and/or compassion fatigue (Alacacioglu et al., 2009; Barnard et al., 2006; Corso, 2012).
Aware of these issues, oncology nurses have devised various coping strategies such as peer support, relaxation methods, personal/group reflection sessions, and positive personal/professional relationships (Florio et al., 1998; Huock, 2014; Wenzel et al., 2011). As with many groups of highly stressed people, certain coping methods can be more damaging to health. The use of alcohol and other substances to reduce stress has been reported in this population (Wallace et al., 2009), which have negative implications for work productivity and the individual’s physical and psychological health. Other problematic consequences can include increased absenteeism (van Mol et al., 2015), and in many cases, highly stressed staff leaving their job prematurely (Bourdeanu et al., 2020; Wells-English et al., 2019), further increasing the problematic nurse shortage (Barrett & Yates, 2002). Consequently, staff shortages have a knock-on effect on job satisfaction and burnout in oncology nurses (Toh et al., 2011).
Support packages and interventions to reduce stress are essential to good organisational functioning, but previous work suggests that oncology nurses are not provided with sufficient opportunities to participate in these, especially for compassion fatigue (Aycock & Boyle, 2009). Occupational health settings are increasingly emphasising preventive initiatives in the workplace. In the UK context, for example, there has been promotion of psychological health in National Health Service (NHS) staff in recent years (Boorman, 2009). Efforts to better understand predictors and experiences of chronic stress in oncology nurses are vital to this effort, as they can negatively impact on the standard and safety of patient care (Kumar & Bhalla, 2019; Zadeh et al., 2012).
Within the occupational stress literature, intervention packages can be categorised based on whether they are person-specific or organisational in nature (Reynolds, 2000). Person-specific interventions address those stressors specific to the individual, and the coping strategies used to combat these. Organisational packages target different aspects of work structure, such as teamwork, managerial responsibilities, caseload distribution, health and safety, and promotion of work-life balance.
A previous review of stress management interventions for general nursing samples (Mimura & Griffiths, 2003) identified that few intervention programmes are based on theoretically derived models or developed in response to specific stressors faced by nurses. They emphasise that future research should provide conceptual clarity about how and why interventions are developed. This is an important context in considering our review of the interventions which follow. To our knowledge, there is currently no detailed review of oncology nurse stress management interventions: we propose that such a review is especially important if we are to develop effective, theoretically driven interventions for this population. In undertaking such a review, we aim particularly to explore how Acceptance and Commitment Therapy/Training (ACT) may be a viable theoretical framework – as an alternative to the existing evidence base – given its conceptual fit and broader evidence base.
REVIEW METHODS
We undertook a narrative review of stress management intervention research in oncology nurses published over the past 15 years. Criteria for article inclusion stipulated that the work had to be: (i) empirically based (i.e. testing the effectiveness of an intervention), (ii) inclusive of a target sample of oncology nurses, and (iii) in the context specifically of occupational stress management outcomes. Nine empirical studies were thus identified. These studies were organised and discussed according to the type of intervention (i.e. educational or psychotherapeutic). Despite the prevalence of stress, surprisingly, few intervention studies have been recently published.
The second half of this paper offers a narrative review of the ACT framework and its potential utility for oncology nurse stress management. Additional literature on the use of ACT in different populations is provided to supplement this work.
INTERVENTIONS TARGETED AT IMPROVING ONCOLOGY NURSE STRESS MANAGEMENT
Using Reynold’s (2000) dichotomy, published studies in the oncology nursing setting appear to use person-specific approaches (e.g. educational workshops, team-based development programmes, and psychotherapeutic approaches), typically in group-format delivery. This is likely due to the feasibility and cost efficiency of person-specific packages over organisational approaches, of which the latter generally require more resources and changes to infrastructure (Reynolds, 2000).
INTERVENTION EFFECTIVENESS: WHAT DOES THE CURRENT EVIDENCE DEMONSTRATE?
Table 1 provides the key details from the studies investigating stress management interventions for oncology nurses. Onan et al. (2013) and Udo et al. (2013) both tested group-based educational interventions, reporting improvements in work-related stress levels, with Onan et al.’s (2013) participants also reporting significantly improved levels of emotional exhaustion after training. Only the effects on work-related stress were maintained to one-month follow-up, but unfortunately no control condition was included for comparison in Onan et al.’s (2013) study design. For Udo et al.’s (2013) findings, the decreased stress levels were related to workload and less feeling of disappointment at work, but the effects were not statistically significant. Le Blanc et al. (2007) and Kravits et al. (2010) also used education-based interventions to target reduction in emotional exhaustion and depersonalisation. Both studies reported significant improvements in both outcomes, but only Le Blanc et al.’s (2007) study reports medium to high effects on emotional exhaustion being maintained at 6-month follow-up. Further, out of the education-based interventions in this review, only Le Blanc and colleagues (2007) include a wait-list control condition, allowing for their findings to account for regression to the mean and potential confounding variables. Kravits et al. (2010) do not provide an interpretation of the strength of the effect sizes, and neither study includes process measures to examine whether their chosen intervention content is responsible for the reported changes in outcome scores. There were also post-intervention reports of reduced personal accomplishment in Kravits et al.’s (2010) study, which is surprising given that they improved scores of emotional exhaustion and depersonalisation. The authors note that this may be due to participants feeling more comfortable reporting their true feelings of personal accomplishment after the intervention, leading to the observation of lower scores, though no supporting data (e.g. qualitative feedback) are presented to corroborate this claim. Compassion fatigue and burnout were the focus of Potter et al.’s (2013) research. Although scores in these outcomes improved after the intervention, and were further reduced at six-month follow-up, only compassion fatigue scores showed a significant improvement from baseline to six-month follow-up. No effect on burnout was observed at any time-point.
Table 1
Intervention studies investigating stress management for oncology nurses
Taking a more psychotherapeutic stance, Cohen-Katz et al. (2005) tested a mindfulness-based stress-reduction intervention (MBSR), reporting significantly improved emotional exhaustion which was maintained at the three-month follow-up. However, no significant improvement in depersonalisation was reported, implying that MBSR has limited effects on this sub-construct within burnout. The clinical utility of the findings is also limited due to no effect sizes being reported in the study. Duarte and Pinto-Gouveia (2016) also tested MBSR and reported post-intervention effects on stress, burnout and compassion fatigue; the effects were medium to large, but no longer-term follow-up was included in the study design. This can make one question the applied relevance of these findings (e.g. providing an arguably lengthy intervention to time-limited nurses) due to the lack of indication for maintenance. Interestingly, however, Duarte and Pinto-Gouveia (2017) did later report that improvements in stress, burnout and compassion fatigue were statistically mediated by changes in psychological inflexibility; we will come to the relevance of this finding shortly.
Villani et al. (2013) successfully improved anxiety levels and coping skills through a mobile phone delivered Stress-Inoculation Training intervention. Scores were not assessed at follow-up, but pre-to-post intervention scores were statistically significantly improved compared to control participants. This study did not, however, include an explicit outcome measure of stress, which seems a curious design choice given the focus of this work. Poulsen et al.’s (2015) study also lacks an explicit stress outcome measure(s); however, significant improvements were observed in recovery experiences (relating to relaxation, self-control, psychological detachment and mastery), satisfaction with general self-care practices (presumedly physical and psychological self-care, though this is not clear), and perceived sleep quality. Medium effect sizes across all outcomes were maintained at six-week follow-up. The applied relevance of these findings to oncology nurse stress management specifically is, however, limited due to the selection of proxy outcomes.
In summary, the intervention studies described above and in Table 1 have reported varied findings across a range of outcomes, but the overall picture is not an entirely clear or conclusive one. Three out of the nine studies did not include measures that target important stress-related concepts (e.g. burnout and compassion fatigue), and so their applied relevance to stress management remains somewhat ambiguous. From this sample of studies, psychotherapeutic interventions seem to produce the most promising results, and they are also methodologically stronger given that: (i) all of them include control groups in their design; (ii) interpretation of effect sizes is more frequently reported (2 out of the 4 studies presented effect sizes); (iii) none of the studies testing psychotherapeutic interventions report negative effects (e.g. the reduced personal accomplishment scores observed in Kravits et al.’s (2010) educational intervention); and (iv), they generally include process measures to determine whether the intervention is performed as intended, allowing us to probe for the mechanisms leading to change in primary outcomes. This final point is particularly important in intervention research, especially in the current zeitgeist of process-based interventions (Hofmann & Hayes, 2018). However, even in those cases where improvements are observed, the lack of follow-up in three out of nine studies (e.g. Duarte & Pinto-Gouveia, 2016; Villani et al., 2013) often renders us unable to conclude whether the reported salutary effects last beyond the intervention sessions.
WHY ACT MIGHT BE A HELPFUL ALTERNATIVE
We were not surprised to find a small number of mindfulness-based intervention studies given that these have also been widely used for stress management in non-oncology nursing populations (Craigie et al., 2016; Delaney, 2018; Foureur et al., 2013; Lomas et al., 2018; Mackenzie et al., 2006; Watanabe et al., 2019). However, previous research has shown that mindfulness-based interventions may have limited long-term effectiveness for stress management in general populations, and in some instances are equally as effective as other approaches such as relaxation programmes (Chiesa & Serretti, 2009). An approach which builds on this limited effectiveness base, with the addition of other therapeutic processes as part of a broader intervention framework, might, therefore, be a wise starting point. For example, creating a drive to want to manage stress via the appetitive function of values-based processes (e.g. clarifying the importance of self-care as a motivator to engage in stress management behaviours), as seen in ACT (Hayes et al., 2011), may function to promote longevity of the intervention effect by increasing engagement in stress management skills (such as mindfulness) in the long term. Mindfulness-based skills may produce short-term benefits, but commitment to values could make participants feel more inclined to engage with the skills beyond the training – a hallmark of long-term behavioural change. The appetitive nature of values selected by clients make them intrinsically rewarding; thus engaging in values-congruent behaviours (e.g. self-care) would be reinforced and, over time, become more fluent (Luoma & Platt, 2015). Values-based processes are not targeted in traditional MBSR, thus justifying the use of more complex, theoretically grounded, intervention approaches.
ACT, being one such framework, is informed by Relational Frame Theory (Hayes et al., 2001), thus having a strong evidence base for including specific intervention components. ACT explores how verbal (thought) content and cognitions can maintain an individual’s negative behaviour and thoughts. ACT has been investigated across many different contexts, including (but not limited to) therapy for psychopathology (Powers et al., 2009; Ruiz, 2010), interventions for health behaviour change (Forman et al., 2009; Heffner et al., 2003; Hernández-López et al., 2009; Lillis et al., 2009) and, specific to this review, for stress in the workplace setting (Dahl et al., 2004; Flaxman & Bond, 2010b). Although ACT has been promoted as suitable for use in the cancer setting (Hulbert-Williams et al., 2015), its application typically focuses on patients rather than care staff.
ACT aims to promote psychological flexibility, i.e. the ability to fully contact the present moment, and the thoughts, feelings and emotions it contains in a non-judgemental manner, and to continue or alter behaviour in pursuit of values-based living (Hayes et al., 2011). Psychological flexibility is widely identified as crucial in the maintenance of healthy psychological wellbeing, especially within a work context (Lloyd et al., 2013; Puolakanaho et al., 2020). It is a means to overcome the detrimental effects of experiential avoidance – the attempt to avoid negative private events (e.g. feelings, emotions, thoughts etc.), even when doing so can lead to behavioural complications in the long run (Hayes et al., 2011). Experiential avoidance is argued to both increase and maintain psychological distress, and negatively influence effective behavioural activation (i.e. engagement in activities which improve mood) (Kashdan et al., 2006).
Experiential avoidance is identified as a risk factor within the workplace and should be targeted in preventive interventions (Bond & Donaldso-Feilder, 2004). Significant medium positive correlations have been found between experiential avoidance and depersonalisation and emotional exhaustion in Spanish critical care nurses (Iglesias et al., 2010), and post-traumatic stress symptoms in palliative care staff (O’Mahony et al., 2015). The Experiential Avoidance in Caregiving Questionnaire (Losada et al., 2014) illustrates the awareness of this concept in the healthcare field. ACT is, therefore, recommended as a promising preventive strategy (Biglan et al., 2008), since the promotion of psychological flexibility is the key outcome. Nonetheless, ACT is not currently being widely used as a stress management approach in oncology caregiving populations. In our scoping searches, we identified only one intervention study that tested ACT for oncology nurses. Habibian et al. (2018) delivered a group-based ACT intervention (four 1.5-hour sessions) to 60 paediatric oncology nurses and special disease nurses (intervention condition, n = 30; control group, n = 30) using a randomised controlled trial (RCT) design. The control group received ‘communication skills’ that were unrelated to ACT, but no further details on this content were provided. Significant improvements were found in job stress scores compared to controls, with these large effects being maintained at three-month follow-up. However, no significant improvements in burnout were found for either condition after the intervention. Surprisingly, no process measure was included, making it impossible to determine whether the theorised intervention processes had a causal effect on the observed improvements in stress.
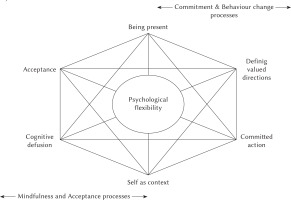
ACT can be presented visually using the ‘Hexaflex’ model (Figure 1). To briefly summarise, six core processes are theoretically linked to one another with the aim of promoting psychological flexibility (Hayes et al., 2011). It is important to note that each core process is considered a positive psychological skill – a technique aimed at helping participants engage with both positive and negative internal content to promote mental wellbeing – and not merely a method to avoid or reduce symptoms of psychopathology.
Figure 1
Acceptance and Commitment Therapy, illustrated using the Hexaflex model (adapted from Hulbert-Williams et al., 2015).
Cognitive defusion is defined as a process which allows an individual to create a context in which their present thoughts and feelings do not excessively regulate their actions or behaviour (Hayes et al., 2011). In a ‘defused’ state, goals and values can exert more control over behaviour, compared to a ‘fused’ state where emotional content exerts control over behavioural activation. For example, a nurse could narrate the different thoughts that flow through their mind after a difficult patient experience in order to create some ‘psychological distance’ between themselves and the thoughts. Self-as-context is an awareness of one’s own experiences (past and present) without attachment to them – in a way, defusion applied to self-concept. This allows an individual to understand their role as an observer to thoughts and emotions, rather than allowing these experiences to contain them and define their self-concept (Hayes et al., 2011). One might use the ‘Classroom metaphor’ (Stoddard & Afari, 2014) to illustrate this, whereby the school classroom is the container of our different positive and negative internal content (depicted as pleasant and ill-disciplined students), as well as the critical or praising approach we have towards that content (i.e. the ‘teacher’ role). The classroom is the perspective we can take in self-as-context, whereby we are simply the vessel in which those experiences occur, allowing one to observe experiences without judgment.
Contact with the present moment through mindfulness training is central to ACT. Mindfulness is a process of purposely paying attention to the present moment (e.g. what a person can see, hear, touch, etc.), including to those aspects of the human experience – thoughts, emotions and so forth. Often when we are feeling stressed, our cognitive attention is focused more on future worries or rumination over past experiences; our emotional state is tied to that worry in a subjectively appraised way that might bring distressing feelings of guilt or self-blame. Mindfulness training offers the ability to know when their conscious attention is not focused on present-moment experiences, and tools to then return it to that state of being in a non-judgmental manner (Kabat-Zinn, 1990). In ACT, mindfulness is a crucial skill to then allow for the training of an Accepting mindset. Often defined as the opposite of experiential avoidance, this state of being is where we train clients to be fully accepting of present moment experiences, even when these might not be desirable. Mindfulness can often feel very easy when the content of the present moment is pleasant and desirable, but when internal content is more personally challenging, there is an increased drive towards experiential avoidance. Acceptance training offers techniques to appreciate that distressing psychological content is just as important to the human experience and should equally be approached and experienced in this non-judgemental manner (Hayes et al., 2011). In oncology nursing, this might involve being open to and exploring not just the patient’s distress regarding illness or death, but also noticing the distress that they themselves can experience.
Values are defined as “ongoing patterns of activity that are actively constructed, dynamic, and evolving” (Wilson et al., 2010, p. 252) that individuals can work towards, and which may facilitate goal setting. A common shared value for oncology nurses might be ‘compassion’, which provides an overarching purpose to the patient care they provide. At the technical level, values are verbally constructed ‘rules’ that motivate an individual to act in a way that is meaningful to them and are especially important in supporting continued action (rather than avoidance) in the state of psychological suffering. In a related psychological process, where an individual makes choices (day-today or larger life goals) in a way that is congruent with their personal values, they are more likely to recognise that their lives have ‘meaning’ (Plumb et al., 2009). After an individual clarifies values for different areas of their life, the final component of ACT is to train skills which encourage a client to pursue or ‘commit’ to specific actions (e.g. clearly communicating empathy in the presence of a distressed patient) that will help bring those values to life – a process called committed action.
PSYCHOLOGICAL FLEXIBILITY AND ITS RELEVANCE TO THE ONCOLOGY NURSING SETTING
Richardson et al. (2015) demonstrated the empirical link between cognitive fusion and self-compassion in USA-based medical students (n = 52): a significant medium negative correlation was reported between cognitive fusion and self-compassion. By promoting cognitive defusion, therefore, ACT interventions have the potential to increase self-compassion, which is known to improve psychological health (Neff et al., 2007), and has relevance to healthcare settings by improving standards of patient care (Wiklund Gustin & Wagner, 2013). In a similar, UK-based cross-sectional study, cognitive defusion negatively correlated with perceived stress, burnout and compassion fatigue, with moderate-to-strong effects, in a sample of 142 National Health Service-based nurses (Kent et al., 2019). Furthermore, all of the ACT processes together accounted for large proportions of variance in perceived stress, burnout, compassion fatigue and compassion satisfaction (R2 range = .36-.61), above and beyond that explained by demographic or work-related variables (e.g. relationship status or years or experience). Acceptance, mindfulness and values-based processes were frequent independent contributors to the variance explained in these chronic stress outcomes, highlighting their importance in nurse-focused stress management interventions. Self-as-context was also significantly predictive of lower perceived stress, but was not a significant predictor for burnout or compassion fatigue. Despite this, self-as-context may still be an important stress management component; for example, nurses who are fused with a self-as-content narrative that they should be able to cope with stress because they are caring and compassionate people (for others) may be more at risk of suffering the negative effects of stress. Fusion with this self-content may consequently lead to minimisation of the stress experience or a reluctance to seek help, which, in the long term, may elevate risks for chronic stress. Cognitive defusion techniques may help by providing separation between this self-as-nurse narrative, and the experiencing self in the present moment (i.e. noticing thoughts and feelings as a conscious stream of events and being guided by one’s values). It is worth noting that relationships between therapeutic process predictors and these various outcomes likely have a temporal element: addressing levels of perceived stress first may in turn help to reduce risks of developing burnout and compassion fatigue, though this requires longitudinal investigation.
Acceptance has been reviewed in relation to coping strengths in informal caregivers of patients with terminal illness and dealing with bereavement (Davis et al., 2015): two issues relevant to the oncology setting. Davis and colleagues (2015) proposed an ACT-based model for volunteer caregivers specifically aimed at acceptance of unwanted thoughts/feelings associated with grief and fear of death, and addressing communication difficulties. Volunteer caregivers have been found to report similar stressors to employed oncology nurses (Hulbert & Morrison, 2006); thus these ideas have applications to this population. Acceptance skills could help oncology nurses to engage in effective care and communication, even in the presence of their own and patients’ suffering (da Fonte Sousa Gomes et al., 2013). Where acceptance is lacking, nurses may instead avoid present-moment experiences of the more distressing parts of their job in the misguided assumption that this will reduce its vicarious effects. Given that this is a known risk factor for compassion fatigue development (Figley, 1995), intervention strategies that overcome this kind of experiential avoidance are hugely important.
Various research supports mindfulness as an effective component in nurse stress management (Bazarko et al., 2013; Mackenzie et al., 2006). Cohen-Katz et al.’s (2005) and Duarte and Pinto-Gouveia’s (2016) studies reviewed previously demonstrate the utility of mindfulness for oncology nurses. Comparatively, a mindfulness-based intervention incorporating values-clarification exercises has been investigated for burnout, depression and post-traumatic stress in USA-based palliative care professionals (n = 17; Gerhart et al., 2016). Significant reductions were found for depressive symptoms and depersonalisation, demonstrating large effect sizes, but no control group was included for comparison, and no follow-up was implemented to explore the maintenance of effect. Importantly, however, significant reductions in cognitive fusion and experiential avoidance were also present, providing tentative evidence for these processes as potential mechanisms of change. The importance of compassion identity in oncology nurses (i.e. evaluating internal coping resources for the stress of caring for the chronically ill and dying; Corso, 2012) has been examined with regards to mindfulness. From an ACT perspective, we might define this as using mindfulness skills to defuse from both fixed coping methods and a fused self-identity to develop self-as-context. Corso (2012) identifies mindfulness as crucial to oncology nurses’ role, as they require constant self-awareness and monitoring of their compassion identity. By freeing up an oncology nurse from ‘fusion’ and allowing development of this compassion identity, not only may stress be reduced, but it may also allow an oncology nurse to attend to each patient’s unique needs more effectively, improving the standard of care provided (Raab, 2014).
Cross-sectional research with Chinese oncology nurses indicated that perceptions of a nurses’ role being important and valuable is related to improved job satisfaction and lower scores of burnout (Cheng et al., 2015). This observation may be amplified through deliberate use of values clarification in intervention studies. Raingruber and Wolf (2015) assessed the unique role of oncology nursing, identifying three main themes involved in sustaining these health carers: (i) importance of vulnerability and thankfulness in patients, (ii) feeling of being spirituality associated with oncology nursing practice, and (iii) the value of being in the moment and recognising priorities as meaningful aspects of oncology nursing. These themes naturally align with an ACT-informed definition of values. A similar finding was reported by Van Rooyen et al. (2008): oncology nurses and their patient(s) were found to develop a special connectedness, requiring them to approach both death and illness directly. Doing this effectively requires the nurses to engage with this psychologically challenging content, and in doing so, might require reflection on their own values, meaning and purpose. Although often done for patient benefit, this psychological work might also benefit the oncology nurse by providing an additional stress management coping mechanism (Van Rooyen et al., 2008).
ACT may, therefore, be even more suited to addressing chronic stress in oncology nurses compared to other purely mindfulness-based approaches (e.g. MBSR or Mindfulness-Based Cognitive Therapy) because of its added emphasis on values-driven behaviour. Values enable an individual to endure stress and other sources of psychological suffering (Bond et al., 2006), and so present a pertinent intervention target. In preventing compassion fatigue in oncology nurses, Corso (2012) suggests that interventions should train participants to “pay attention to the people and activities that nurture your mind, body and spirit. Commit to making time to increase those interactions or activities” (Corso, 2012, p. 449). Corso is not writing from a pro-ACT perspective, but the links between this quote and the committed action component within ACT are clear.
Based on this literature, we suggest that the core features of the ACT model make it highly relevant to the context and nature of the oncology nursing environment. Burnout prevention approaches which focus on the relationship between the individual and the situational stressor have long been considered as most effective (Maslach & Goldberg, 1998). ACT does so by modifying how an individual relates to their environment and experiences, rather than attempting to change or reduce the stressor. This is an important outcome goal given that the frequent stressors reported by this group are often not changeable; it thus makes sense to instead intervene on how one responds to (a) the presence and (b) the non-changeability of those stimuli (Blackedge & Hayes, 2001). This reconceptualization of stress appraisal offers a more workable approach compared to an ‘avoidant’ stance to dealing with stressful situations (Butts & Gutierrez, 2018), which are, in most cases, unavoidable as part of the job.
ACT implements a ‘unified model’ (Hayes et al., 2011), in that all of the components theoretically interact to increase psychological flexibility. Consequently, ACT protocols are likely more participant-friendly as each exercise or session naturally leads on to the other (e.g. the importance of firstly adopting an open and accepting approach to internal content in order to more effectively focus on the present moment; Flaxman et al., 2013). This allows for a more comprehensive understanding of the different stress management skills which may help to avoid participant attrition (Richardson & Rothstein, 2008). Encouragingly, and perhaps consequently, a meta-analysis published last year reported that dropout rates were lower for ACT interventions (17.35%) compared to comparison conditions (18.62%) (Karekla et al., 2019). ACT has been widely developed in group and/ or brief format (Strosahl et al., 2012), for example, web-based interventions, and 1-2 hour workshops. This could be a suitable solution for oncology nurses who regularly face barriers to research participation, such as workload (Roxburgh, 2006). ACT is amenable to delivery through coaching (e.g. skills training rather than ‘therapy’; Hulbert-Williams et al., 2016), which may make participation in interventions more acceptable and less stigmatising. Furthermore, there is now an abundance of process measures that allow for evaluation of the different components within intervention studies; of all available theoretical frameworks for psychological interventions, this model thus lends itself to a greater extent to high quality designs incorporating mediation and process modelling of intervention components. Examples include the work-related Acceptance and Action Questionnaire (Bond et al., 2013) to measure psychological flexibility in a work context, or the Valued-Living Questionnaire (Wilson et al., 2010) to measure the values component.
ACT INTERVENTIONS FOR EMPLOYEE WELLBEING IN NON-ONCOLOGY HEALTHCARE SETTINGS
That there was only one study on ACT for oncology nurses surprised us. However, a further rationale for the use of this framework can be found in the evidence in other organisational contexts (Bond & Bunce, 2000; Flaxman & Bond, 2010a, 2010b). Research in the healthcare professional setting is still limited, though there are relevant studies testing benefits for various groups in the caring professions. For example, using an observational design, Pakenham (2015) investigated cross-sectional correlations between ACT processes (values, acceptance, mindfulness, thought suppression) and adjustment outcomes (e.g. stress and psychological distress) in clinical psychology trainees (n = 116): higher scores on acceptance and values measures, and lower scores on thought suppression, were each related to lower work-related stress (small effects) and psychological distress (small effects).
Two RCTs of ACT with qualified (O’Brien et al., 2019) and student nursing samples (Frögéli et al., 2015) reported significant reductions in mental health symptoms (medium effects), perceived stress (large effects), and burnout (large effects) when compared to both wait-list and treatment-as-usual controls. The lengthy follow-up in Frögéli et al.’s study (2015) allowed them to further demonstrate that improvements in perceived stress at one-year follow-up were significantly mediated by change in experiential avoidance during the intervention (i.e. from baseline to the end of the sixth session), indicating that the effects lasted well beyond the training sessions (Frögéli et al., 2019). O’Brien et al. (2019) found that their nurses reported significantly fewer days (medium effect size) missed due to injury (e.g. musculoskeletal complaints), implying that ACT has potential positive implications for both the psychological and physical health of nurses.
Brinkborg et al.’s (2011) ACT RCT with 106 Swedish social workers found that, compared with wait-list controls, a significant difference was found in those participants who presented high stress at baseline (> 25 on the Perceived Stress Scale), with 42% of the intervention condition showing clinically significant post-treatment change (i.e. classified as ‘recovered’ and defined using a cut-off point supplemented by Swedish norm data on stress levels), compared to only 11.5% of the control group. This was coupled with statistically significant improvements in burn-out and general mental health. Similarly, McConachie et al.’s (2014) study with intellectual disability support staff found significantly reduced distress (medium-to-large effects) and thought suppression (medium effects) in their ACT intervention participants compared to wait-list controls, with more pronounced effects being observed in those participants presenting higher psychological distress at baseline (i.e. six weeks before post-intervention measures). These findings concur with Reeve et al.’s (2018) meta- analysis of ACT for burnout in mental health professionals, which concluded that ACT is particularly useful for those staff members who present high levels of distress at baseline. This means that, even for those participants at greater risk of chronic stress and other related variables (e.g. distress), ACT is likely to produce salutary effects of clinical significance.
Importantly, the use of ACT process measures allowed the researchers to examine whether intervention effects were mediated by changes in the underlying theoretical components being targeted. For example, Frögéli et al.’s (2015) study demonstrated that increases in psychological flexibility and mindfulness were distinctly predictive of decreases in perceived stress and burnout scores in their student nurse participants. McConachie et al. (2014) reported a significant reduction in thought suppression between post-intervention and follow-up observations in their intervention group, leading to decreased reduction in psychological distress. This latter finding is especially important as thought suppression is actively encouraged in some other intervention frameworks (e.g. traditional CBT approaches), suggesting that these may actually increase the risk of work-related distress.
IMPLICATIONS FOR FUTURE RESEARCH
The stress management interventions for oncology nurses discussed herein offer varied results, with the overall picture not being entirely clear or conclusive. Psychotherapeutic interventions appear to provide the most promising results compared to educational approaches, in terms of efficacy and methodological robustness. A comprehensive review of this literature would not be complete without a critical review of the methodology. Word space precludes us spending too much time on this; however, there are some important limitations in previous work that are worth highlighting and considering for future study design.
LESSONS TO BE LEARNED: METHODOLOGICAL LIMITATIONS OF CURRENT INTERVENTION STUDIES
Firstly, the general under-reporting of effect sizes across the literature considerably hinders both the interpretation and applicability of intervention findings. Stress management interventions aim to be both preventative and reactive. Thus, to effectively demonstrate these qualities, studies must report long-lasting intervention effects (i.e. robust effect sizes of clinical significance at follow-up). Such effects would imply that participants learn to use self-care skills and incorporate them beyond the duration of the study: a hallmark of lasting behaviour change. However, we recognise that the interpretation of these effect sizes may be confusing due in part to the variability in reporting effect sizes, and the different (or lack of, e.g. Duarte & Pinto-Gouveia, 2016) follow-up periods and outcome measures which are incorporated across studies.
Control groups are an important quality indicator for intervention research (Street & Luoma, 2002). They can be used to (i) examine if an intervention affects a desired outcome beyond what would naturally occur over the course of the study; and (ii) to establish that changes in the outcome are not caused by extraneous variables associated with the participant (e.g. capability to deal with the problem, or readiness to change) (Street & Luoma, 2002). Whilst some studies on stress management for oncology nurses use control conditions, many tend to be either wait-list groups (Cohen-Katz et al., 2005; Duarte & Pinto-Gouveia, 2016) or control groups which received no ‘intervention’ at all (e.g. Le Blanc et al., 2007). Some studies report greater effects in their intervention than the mere passage of time (i.e. a wait-list group), but it is often difficult to measure what specifically is happening for the control group, making comparisons between the conditions difficult. Only a small handful of studies reviewed here (e.g. Habibian et al., 2018; Poulsen et al., 2015; Udo et al., 2013; Villani et al., 2013) used active control groups – conditions which received ‘neutral’ exercises/sessions, often referred to as ‘psychosocial placebos’ – and it is these studies which are able to demonstrate greater control over non-specific factors (e.g. therapist competence), thus concluding with more confidence that differences in observed outcomes between the groups are more likely due to the intervention effects (Street & Luoma, 2002).
Intervention length is an important consideration too; attrition rates are typically higher in longer intervention studies, which can lead to potential bias, and have detrimental effects on the internal/external validity of results (Barry, 2005). In the current literature, many of the studies report attrition rates (though Villani et al., 2013 did not), and most of these are relatively low (e.g. n = 4 in Cohen-Katz et al., 2005), even when their intervention could be considered lengthy in this setting (eight 2.5-hour weekly sessions in Cohen-Katz et al.’s, 2005 case). Some studies, however, do report higher attrition rates, which becomes especially problematic where baseline sample sizes are also small (e.g. Onan et al., 2013; Poulsen et al., 2015; Udo et al., 2013). Whilst explanations for their attrition rates are often provided, some of which cannot be controlled for (e.g. maternity leave; Onan et al., 2013), the majority are due to incomplete data sets and/or participants not completing all of the intervention sessions. This is likely due to busy work schedules (Walczak et al., 1994), which, although reasonable, leaves little room for statistical control of these potentially confounding effects. This further emphasises a need for briefer intervention packages in the future. ACT is useful in this context due to its versatility (e.g. group-based delivery; Walser & Pistorello, 2004) and ability to produce promising effects with intervention packages as brief as 1-2 hours (see Strosahl et al., 2012 for a detailed overview).
Many published interventions do not use (or clearly justify and explain) empirically validated principles or frameworks which inform intervention components. This is especially the case with educational interventions (e.g. Le Blanc et al., 2007; Poulsen et al., 2015; Udo et al., 2013), compared with psychological interventions (e.g. Cohen-Katz et al., 2005; Habibian et al., 2018). The former generally lack a detailed rationale for how that intervention package has been constructed (i.e. justification for why the different components and exercises are included in the protocols), an issue raised almost two decades ago that seems not to have since been improved (Mimura & Griffiths, 2003). Comparatively, Cohen-Katz et al. (2005) and Duarte and Pinto-Gouveia’s (2016) use of MBSR is well described and justified through presentation of the MBSR model, and previous evidence in similar populations. Of course, it is difficult to know whether this is a problem of the study design per se, or of word limitation imposed in journal reporting. As mentioned previously, ACT is an empirically validated framework (Hayes, 2016), with individually defined components which can be applied to numerous contexts and needs (i.e. a transdiagnostic approach; McHugh, 2011). This makes ACT a suitable method to address the issues previously raised by Mimura and Griffiths (2003). We recommend that future studies in this context appropriately describe how their ACT intervention is designed for the target population and needs.
In addition to reporting why certain intervention components are included, it is advantageous that study designs include measurement of process change to examine whether the intervention is affecting change in the way it is designed to. This knowledge further increases understanding of the components that possibly promote the effect, and which can be built upon in subsequent research to promote those aspects more effectively (Levin et al., 2012). Few published studies using educational intervention frameworks include such measures, which makes it difficult to confidently state whether the observed effects are due to the content of those interventions. In comparison, studies using psychological interventions generally provide a more data-driven approach to intervention design and testing. For example, Duarte and Pinto-Gouveia (2016) assessed change in mindfulness using process measures and how this relates to outcome improvement (e.g. mediation analysis; Imai et al., 2010). This methodological approach concurs with the recent paradigm shift towards process-based therapy in intervention research (Hofmann & Hayes, 2018). Not assessing processes of change also impairs our ability to refine interventions over time, or to distil them to their most impactful components. Given the time pressures for intervention delivery, information as to which processes should be preferentially targeted would be valuable to maximise effectiveness. In this review, neither Villani et al. (2013) nor Habibian et al. (2018), who each tested psychotherapeutic interventions, included process measures. The latter case is especially surprising given the abundance of psychometrics offered by the ACT literature to assess process change (Levin et al., 2012). We therefore recommend that all ACT-based research in employee stress management ensure that validated process measures are included in its methodology.
To further illustrate the importance of specifying and measuring intervention components, a meta-analysis of 55 occupational stress intervention studies including over 2400 participants across various settings (including nursing and hospital contexts) found that cognitive-behavioural programmes produced larger effects compared to other interventions, for example, relaxation and organisational interventions (Richardson & Rothstein, 2008). However, the authors concluded that the more complex and lengthier the intervention, and as more components are added, the poorer the improvement in stress, as this often confuses and overwhelms participants (Richardson & Rothstein, 2008). This therefore makes the tailoring of intervention content an important process. Previous research revealed that participants perceive that tailored interventions make it easier to remember the information provided, allowing one to apply the techniques outside of the training environment more effectively (Ryan & Lauver, 2002). Nonetheless, the lack of intervention tailoring continues to permeate the literature. Habibian et al. (2018), for example, did not implement a tailored manual in their study but instead used an ACT intervention (Bach & Hayes, 2002) originally designed for hospitalisation prevention for patients diagnosed with psychosis to guide their content. This might have made it difficult for participants to understand how the ACT-based skills could be applied to their specific setting and experiences, which may, in part, explain the lack of effect on burnout scores observed in their study. Understanding the mechanisms of effect within an intervention allows one to develop tailored, data-driven interventions, and is a pertinent step is avoiding the issues raised above by Richardson and Rothstein (2008). In the context of nurse stress management, our recent empirical research (Kent et al., 2019) recommends that ACT interventions prioritise acceptance, mindfulness and values-based processes, as these appear to have the most potential in demonstrating beneficial effects for this population.
Whilst research investigates ACT interventions in this context, in the meantime we recommend that employers and health services use current psychotherapeutic stress management interventions which are based on evidence stemming from methodologically robust research (e.g. those that include mediation analyses). In this context, mindfulness-based approaches are growing ever more popular, given the abundance of evidence in the MBSR literature, and are a viable starting point which can be further developed and optimised in the future (e.g. using ACT principles such as values-based living).
CONCLUSIONS
Given the prevalence of chronic stress in oncology nurse populations, there is a clear need for further research testing effective and acceptable interventions. The existing literature reports only a handful of studies which use validated psychotherapeutic models for effective stress management, though it is these kinds of interventions that may produce more reliable, longer-lasting effects. It is plausible to assume that longer-term reduction of stress will act as a preventive strategy for decreasing future risks of burnout and compassion fatigue. Although ACT has only been tested once in an oncology nursing sample (Habibian et al., 2018), there is a conceptual overlap with findings reported in the non-interventional, observational, theoretical modelling work undertaken in oncology nursing samples (e.g. Cheng et al., 2015; Corso, 2012; da Fonte Sousa Gomes et al., 2013). We present a case in this paper that we believe supports the need for further intervention research using this framework, and we have highlighted important methodological limitations in the extant literature that should be considered in the design and implementation of these future studies.


