BACKGROUND
Fatigue in cancer, often described as cancer-related fatigue, is a complex syndrome with diverse causes, covering physical, mental, and emotional components. Patients experiencing it define it as a chronic or abnormal whole-body experience of tiredness, combined with decreased capacity for physical and mental work. This condition is not related (or not proportionally related) to activity and is often less likely to be relieved by rest (Patarca-Montero, 2004). The European Association for Palliative Care defined cancer-related fatigue and underlined the subjective aspect of feeling tired, weak, or lacking energy (Radbruch et al., 2008).
Among cancer patients, fatigue is one of the most troublesome and most frequently reported complaints. The frequency of this ailment is estimated differently depending on the design of the research, specifically the type of the study group, the questionnaire or scale used in the study to measure fatigue, and (connected with it) the theory and definition of fatigue (Donovan et al., 2013).
A more recently published meta-analysis of articles from 1993 to 2020 revealed that the overall severity of fatigue in the group of patients was 49%. Among patients with advanced cancer, the highest intensity of fatigue observed was 60.6%. The authors drew attention to the interesting issue of a decreasing intensity of fatigue in studies, from an average of 64% in publications from 1996 to 2000 to 43% in more recent studies – those after 2016 (Al Maqbali et al., 2021).
A higher intensity of fatigue is observed in patients during treatment, for example during chemotherapy. In a slightly older systematic review of publications on fatigue in patients receiving chemotherapy, it was found that up to 68% of patients experience such fatigue, depending on the studies (Iop et al., 2004). In the already cited recent meta-analysis, fatigue during treatment was reported by 51% to 62% of patients (Al Maqbali et al., 2021).
Furthermore, it seems that fatigue can be a problem even after treatment has ended. The research by Cella et al. (2001) revealed that 33% of patients, even more than 5 years after the end of treatment, experienced at least 2-week episodes of fatigue, which significantly affected quality of life. The influence of fatigue on quality of life can be seen in many other studies. It can be concluded that fatigue is associated with a reduced quality of life for cancer patients (Visser & Smets, 1998) even independently of the effects of age and prior treatment history (Gupta et al., 2007). If the patient cannot find a way to cope with fatigue, it becomes increasingly associated with a wide range of negative effects that stimulate the sensation of losing control of parts of one’s life, with the final result of a “vicious circle” and loneliness, isolation, and further reduction in activity (Flechtner & Bottomley, 2003).
There is also evidence to suggest that fatigue may have a greater impact on daily life than pain in cancer patients while undergoing chemotherapy (Williams et al., 2016). Such data may be surprising, but it might be worth investigating them closely, due to the high awareness of the problem of pain in cancer. In practice, patient care for pain seems to be one of the most important tasks for medical staff. Fatigue is sometimes pushed into the background, disregarded, or considered an unimportant ailment. The same research revealed that 29% of staff noted the impact of fatigue on patients, and 25% of oncology nurses recognized the strength of this phenomenon in the life of their patients (Williams et al., 2016).
Our study pursued several research goals associated with cancer-related fatigue. One of them was the assessment of the prevalence of fatigue in a group of patients undergoing chemotherapy. Another goal was to explore both the understanding of the reason for fatigue and awareness of the ways of coping with it from a patient’s subjective perspective. The main purpose of the study was to compare this subjective perspective of patients with the estimates of medical staff about patient fatigue.
PARTICIPANTS AND PROCEDURE
PROCEDURE
This research project was approved by a university bioethics committee, and the management of the medical facility responsible for chemotherapy also approved the research at the hospital (NKBBN/110). The study included patients eligible for chemotherapy after expressing voluntary consent to participate. A short interview on the perception of patients’ fatigue was also completed by the staff cooperating with the patients – mostly nurses employed in the chemotherapy ward. The study was conducted by a psychologist who was neither part of the team nor employed in the facility.
MEASURES
Author-designed survey (for the patient). The first question in the survey assessed the feeling of fatigue in the past week with possible “yes” or “no” answers. If the answer was “yes”, the next question concerned the assessment of the severity of fatigue using the Numerical Rating Scale – NRS (0 – no fatigue, 5 – moderate fatigue, and 10 – very severe fatigue). The question was followed by other questions about current fatigue, the strongest fatigue, the influence of fatigue on life and the influence of fatigue on quality of life, also using an NRS with answers from 0 to 10.
The next question concerned the main cause of fatigue, which was an open-ended question to which patients answered freely.
Both those who reported feeling tired and those who did not were asked whether they had any ways to deal with fatigue, with possible “yes” or “no” answers. If the answer was “yes”, there was a request to list the fatigue-coping methods and evaluate their effectiveness. In the end, there was an open-ended question about whether and with whom patients discussed their fatigue. All patients’ answers were entered in an open-ended questions format.
Short interview (for the medical staff). The short interview for staff involved three questions. The first was whether the patient seemed to experience fatigue, with possible “yes” or “no” answers. If an affirmative answer was obtained, the medical employee was asked to indicate the severity of fatigue using the same NRS used by the patients (from 0 to 10). The third question assessed possible causes of fatigue in particular patients. The psychologist recorded the answers given orally by the medical staff.
Chalder Fatigue Questionnaire (CFQ-PL). This questionnaire was developed to measure the severity of fatigue among adults in clinical and research settings (Cella & Chalder, 2010; Chalder et al., 1993). It consists of 11 items reflecting a multidimensional view of fatigue, covering decreased mental and physical endurance, fatigability and problems with cognitive functioning connected with increased levels of tiredness. The questionnaire was designed as a self-report measure. Patients answer questions using a four-step scale including better than usual, no more than usual, worse than usual, and much worse than usual. There are two scoring systems; this study used the simpler one connecting the summation of points obtained by each patient. The minimum score in this system is 0, and the maximum is 33 points.
The Polish adaptation of this questionnaire showed very good psychometric values of the tool overall, with satisfactory validity and reliability (Zdun-Ryżewska et al., 2020). The Polish adaptation procedure was carried out in groups of healthy people, and in the present study, attempts were also made to verify the questionnaire in the clinical conditions for which it was originally created.
EORTC QLQ-C30. Approval for the use of the EORTC QLQ-C30 was obtained from the EORTC Quality of Life Group. For this article, only the fatigue subscale was used from the scale. The questionnaire was designed and adapted to measure the quality of life and its various aspects in a group of patients with cancer (Nolte et al., 2019; Waghmare, 2022).
PARTICIPANTS
This study involved 51 middle-aged people, mostly women, who accounted for 67% of the entire group. Of the subjects, 23% reported having no children, while most of the group had children, from 1 to 4. Diverse levels of educational attainment were fairly evenly represented in the group. More than 40% were professionally active, and 57% were retired or disabled. The majority of the surveyed group described their financial situation as “bad” (49%), whereas a significant portion reported their financial situation as “good” (47%). A detailed description of the study group in terms of sociodemographics is presented in Table 1.
Table 1
Socio-demographic characteristics of the study group
Patients who qualified for chemotherapy treatment volunteered for the study. All had been diagnosed with cancer. Nearly half of the group consisted of patients diagnosed with gynecological cancer including breast cancer (49%), while a significant portion of the group had colorectal cancer (13%). The mean duration of the disease was 13 months, and the mean duration of treatment was 7 months. The collected clinical data are presented in Table 2.
Table 2
Clinical characteristics of patients who participated in the study
RESULTS
In this study, patients were asked if they experienced fatigue as a problem (possible answers were “yes” or “no”). Medical staff members were asked to make similar estimations of their patients’ fatigue as a complaint (“yes” or “no” answers could also be given). Four categories appeared in the list of all answers. Patients and staff in most cases agreed on the state of fatigue of the patients (in 63% of cases overall). However, in 37% of the responses, the staff misconstrued the patients’ fatigue or lack of it. This means that in 37% of cases the personnel misdiagnosed the patient’s fatigue (Table 3).
Table 3
Consistent and discordant assessment of patients’ perceived fatigue made by patients and medical staff
Even more discrepant were the assessments of the intensity of patient fatigue made by patients and staff using the 1-10 NRS. In these cases, the Fleiss kappa coefficient of agreement was only 0.13. The mean and standard deviation of fatigue estimated by the patients were M = 4.50, SD = 3.10. For personnel assessing their patient’s fatigue, the mean was M = 3.60, with SD = 2.79.
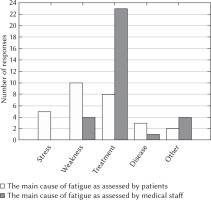
Quite significant differences were also observed between the estimations of the causes of the patient’s fatigue made by the staff and the patient’s own estimations. Patients identified more causes of fatigue, including stress not accounted for by medical staff. The vast majority of the medical personnel viewed the causes of their patient’s fatigue as the “helpful”, but also “burdensome” treatment of cancer. Patients’ answers were quite evenly distributed, with most of them claiming “general weakness” as the main cause of fatigue. Detailed data, including patient and staff responses, are presented in Figure 1.
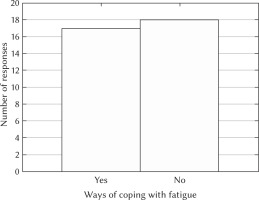
Subsequent questions were posed only to patients and concerned whether they knew of any ways to deal with fatigue and with whom they most often discussed their fatigue. The answers to the first question are presented in Figure 2, which show a fairly even distribution of answers, with a slight increase in responses from people who did not know of any ways to cope with fatigue.
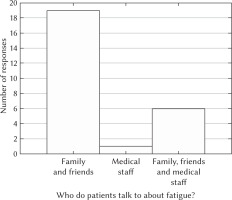
In turn, Figure 3 shows that patients most often discussed their fatigue with family and friends, while only 1 person indicated that the partner in the conversation on this topic was someone who represented the medical staff.
The study also used two inventories to measure fatigue: the Chalder Fatigue Questionnaire and the EORTC QLQ-C30 fatigue subscale combined with NRS fatigue estimations.
The Chalder Fatigue Questionnaire (CFQ), adapted to Polish conditions (PL), was used for the first time in a group of oncological patients. The questionnaire turned out to be a psychometrically valuable tool; the external validity measured by the correlation between the inventories and numerical rating scales was satisfactory:
CFQ-PL and fatigue (EORTC QLQ-C30) rho = 0.56, p < .05;
CFQ-PL and intensity of fatigue (NRS) rho = 0.51, p < .05;
CFQ-PL and average fatigue (NRS) rho = 0.53, p < .05;
CFQ-PL and strongest fatigue (NRS) rho = 0.50, p < .05;
CFQ-PL and influence of fatigue on patient’s quality of life (NRS) rho = 0.51, p < .05.
In addition, both questionnaires and sets of NRSs well differentiated patients both reporting and not reporting fatigue. There were statistically significant differences between these two groups in terms of fatigue measured by the CFQ-PL (a stronger intensity of fatigue was visible in patients reporting fatigue) and the subscale of fatigue from the EORTC QLQ-C30 and all employed numerical rating scales. Detailed calculations made using the Mann-Whitney U test are presented in Table 4.
Table 4
Differences between the group of patients reporting and not reporting fatigue, considering patient fatigue measured by questionnaires
While simple patient declarations in the form of answers to the question whether the patient was tired (“yes” or “no”) corresponded to the results of reliable and accurate questionnaires and simple numerical scales, the staff’s estimations in the form of answers to the question whether the patient was tired (“yes” or “no”) coincided with the results of the questionnaires only in one case, on only one of the NRSs for fatigue (current patient’s fatigue).
Only in this case, the group of staff who answered that they noticed the patient’s fatigue and the group of those who did not report fatigue in the patient’s case differed in the intensity of fatigue measured by the patients themselves using the NRS. In all other cases, there was no difference between the two groups of healthcare workers in the severity of patients’ fatigue as measured by the CFQ-PL and the other scales and questionnaire (average fatigue, strongest fatigue, influence of fatigue on life in general, and influence of fatigue on the patient’s quality of life) (Table 5).
Table 5
Differences between the groups of medical personnel acknowledging and not acknowledging patient fatigue, considering patient fatigue measured by questionnaires
DISCUSSION
The results presented above reveal a certain discrepancy regarding estimations of fatigue in a group of patients and medical staff. Although 63% of the assessments were consistent, the 37% that lacked consistency in the basic assessment of whether the patient is fatigued or not is worrying. Even greater differences were revealed when it came to assessments of the severity of fatigue, where we no longer observed any agreement. The simple question of whether one is tired or not corresponds perfectly with all the questionnaires used to measure fatigue (CFQ-PL, EORTC QLQ-C30 fatigue subscale, NRS current, average, and strongest fatigue) in the group of patients. Patients reporting fatigue differed from those who did not report fatigue in the intensity of fatigue in these questionnaires. Differences between fatigued and non-fatigued patients could also be seen in the case of the NRS concerning the assessment of the impact of fatigue on everyday life and its quality. The group of patients who were fatigued reported a greater impact of this condition on their lives compared to those who were not fatigued.
The question of a simple estimation of whether a patient is fatigued or not, made by medical staff, is completely different in the context of a patient’s subjective, more elaborate answers. Such estimates corresponded to only one numerical scale in which the patient assessed current fatigue. The assessment of whether the patient was fatigued or not was not related in any way to the results of reliable and valid questionnaires to measure the severity of fatigue and other NRSs (average and strongest fatigue and the impact of fatigue on the patient’s life and quality of life) completed by the patients. Such a difference of perspective cited in the literature is unfortunately nothing new. From time to time, studies are published showing discrepancies in assessment, or a misunderstanding of the fatigue experienced by patients on the part of medical staff (Harrington et al., 2023; Piredda et al., 2007). In one of these studies, oncologists were shown to be extremely sensitive to patients’ needs (even more so than those reported by the patients) and showed a fairly thorough insight into the patients’ symptoms, all except for fatigue (Newell et al., 1998). One can also find more optimistic data in the scientific literature indicating that medical staff members recognize the problem of fatigue among patients (even overestimating its impact on everyday life), but such publications are in the minority (Stone et al., 2003).
The authors of a child fatigue scale – namely three related scales for measuring child fatigue: the oncological patient, filled in by the child (the Childhood Fatigue Scale), their parent (the Parent Fatigue Scale) and the oncologist (the Staff Fatigue Scale) – are also convinced of the need to consider different perspectives. Even the very way of defining fatigue may differ among these groups. Children perceive fatigue as overwhelming exhaustion and difficulty moving or opening their eyes. Parents perceive their child’s state of fatigue as a depletion of energy that occurs under the influence of many factors, including the disease itself, nutrition, emotions, behavior, family activities and treatment. Oncologists, on the other hand, define fatigue as a symptom accompanied by an emotional state, combined with withdrawal, mood swings, increased irritability, and depressed mood. Similarly, the perceived causes of fatigue may differ among these three groups (Hockenberry et al., 2003). Our research also revealed a difference in the perception of the causes of fatigue. Medical staff identified chemotherapy as responsible for fatigue to a much greater extent than patients, who gave various reasons for fatigue (including treatment, but it was not the predominant answer). Patients identified more causes of fatigue, including stress, which was not identified by medical staff. From various data collected in a relevant meta-analysis, information can be found that the overall correlation between psychological distress and cancer-related fatigue is stronger than between any other symptoms (Oh & Seo, 2011).
In our study, in the group of patients who gave an affirmative answer to the question of feeling fatigued, as many as 51.4% did not know of any ways to cope with fatigue. Also the majority of the study group did not mention the problem of fatigue to the medical staff. Fatigue is a topic of conversation among friends and family. This is consistent with the results of studies by other authors; for instance, one study showed that 66% of patients did not raise the issue of fatigue in conversation with doctors. Patients identify various reasons for this phenomenon, but one of the main ones is patients’ lack of knowledge about the treatment options for fatigue. Such an answer in the cited study was given by as many as 43% of respondents (Passik et al., 2002). In another, slightly older study, which included three perspectives (those of patients, their caregivers and doctors) in the context of fatigue, as many as 80% of oncologists were convinced that fatigue is an often-overlooked and untreated topic, and the majority of patients (74%) believed that it is something that they just have to endure (Vogelzang et al., 1997). Research points to even more potential roadblocks to bringing the subject of fatigue to the conversation with medical staff for example, starting with the type of cancer, the patient’s religiosity, the impact of fatigue on everyday life or even the fear that talking about fatigue will distract the doctor’s attention (Shun et al., 2009). Some of the roadblocks were identified by the authors of a very useful scale: the Fatigue Management Barriers Questionnaire – adapted for oncological patients (Passik et al., 2002).
CONCLUSIONS
Despite existing recommendations on the need to screen (Fisher et al., 2022) and educate patients in the context of cancer-related fatigue, provided for example by the European Society for Medical Oncology (Fabi et al., 2020), or the US National Comprehensive Cancer Network (Berger et al., 2015), and a huge amount of material on the subject available to the patient and medical staff on the Internet, the issue of fatigue still seems to require attention. In recently published studies, more than half of the surveyed patients (especially the elderly) noted a lack of knowledge and information about fatigue. Across the whole group, 41% of study participants reported that they had not received any questions about their fatigue from healthcare professionals. Of the group that experienced extreme fatigue, only 13% of patients were helped by the medical staff in the form of screening in the context of the intensity of fatigue (Schmidt et al., 2021). With a significant discrepancy in the perception of fatigue between patients and staff, there is a risk that the problem of cancer-related fatigue will go unnoticed. Subjective assessments regarding the state, motivation, and emotions of another person are part of social life which humanistic psychologists and humanistic-existential psychotherapists particularly emphasize. Sometimes we forget too easily how many of our assessment results are derived from our perceptions and do not necessarily correspond to the patient’s condition and feelings. We hope that this study will become part of the important discussion on cancer-related fatigue under the slogan: “Ask the patient. Don’t assume”.
STUDY LIMITATIONS AND FUTURE DIRECTIONS
Our study, although addressing an important topic, is subject to all the limitations inherent in cross-sectional studies. It identifies certain phenomena but does not explain their occurrence or evaluate long-term effects. The participants in our group also comprised a diverse population treated primarily for two types of cancer. However, this does not appear to compromise the study’s conclusions, as we were interested in comparing the perceptions of fatigue between patients and staff independently of diagnosis. Nevertheless, it should be noted in the analysis that the sample size was relatively small, and the study population consisted mostly of women.
An intriguing area for investigation appears to be the exploration of fatigue dynamics within a longitudinal study framework. Tracking fatigue dynamics and related variables throughout the treatment process over an extended period could provide a more comprehensive understanding of this phenomenon.
Additionally, the issue of the associations between chemotherapy as a perceived cause of fatigue, wherein clear differences in patient and staff assessments have emerged, seems worthy of exploration.
Furthermore, investigating barriers that impede discussions about fatigue with medical personnel could prove to be a significant area of inquiry.